AI-Powered Personalized Approach Improves Diagnosis of Heart Condition, Especially for Women
4 Sources
4 Sources
[1]
Why more men than women are diagnosed with deadly heart disease
The research, published in the Journal of the American College of Cardiology andfunded by the British Heart Foundation, details how current guidelines might be changed after showing a new personalised approach improves diagnosis accuracy. When they tested their updated approach in 1,600 patients with clinically diagnosed hypertrophic cardiomyopathy (HCM), the researchers found that it was particularly beneficial for women, increasing identification by 20 percentage points. The new method takes people's age, sex and size into account to determine whether their heart muscle is dangerously large. As well as preventing people being missed, it could also reduce the number of people mis-diagnosed with HCM. Around one in 500 people in the UK have HCM, a genetic condition where the muscular wall of the heart becomes thickened, making it harder for the heart to pump blood around the body. It can cause life-threatening problems like abnormal heart rhythms, which can lead to cardiac arrest and sudden death. Typically, two-thirds of people currently diagnosed with HCM are men, but researchers say women are just as likely to have the condition. There is no single gold standard test used to diagnose HCM. Doctors review a variety of tests and scan results. The most important of these involves measuring the thickness of the wall of the left ventricle, the heart's main pumping chamber. For 50 years the threshold for diagnosing HCM this way has been 15 millimetres for everyone -- if the muscle is thicker than this, a patient is considered likely to have HCM. Dr Hunain Shiwani (UCL Institute of Cardiovascular Science and St Bartholomew's Hospital), who led the research, said: "It is clear that this threshold, which is based on the results of studies from the 1970s, needs to be reconsidered. Having the same cut off for everyone regardless of age, sex or size completely ignores the fact that heart wall thickness is strongly influenced by these factors. "Our research provides a long-overdue update, showing that a personalised approach improves the accuracy of diagnosis. Effective treatments for HCM are starting to be used for the first time, making it more important than ever that we can correctly identify those who need them." The team used an AI tool they developed to analyse MRI heart scans with greater precision and in much less time than a human can. The tool was given 5,000 MRI scans of healthy hearts and measured the thickness of the left ventricle wall in each. From these data, the researchers were able to determine what normal ventricle wall thickness is for people of different ages, sexes, and sizes -- measured by body surface area. This allowed them to set thresholds for abnormal wall thickness, indicating HCM, depending on a person's age, sex and size. The threshold was set higher if the person was older, larger or a man, and lower if they were younger, smaller or a woman. After testing the accuracy of the new thresholds in the group of HCM patients, the researchers applied them, as well as the current 15 mm cut-off, to a group of over 43,000 participants in the UK Biobank. For every eight people identified with possible HCM using the current threshold, only one was a woman. People identified were also much taller, heavier and older than the population average. When the new personalised thresholds were applied instead, the overall number of people identified was lower, suggesting fewer misdiagnoses. Importantly, there was a much more even split between men and women -- with women making up 44% of those identified -- a much more realistic finding since HCM should affect men and women equally. By incorporating other key factors, including ethnicity, and ensuring the new thresholds work with echocardiogram scans, which are more commonly used clinically, the team hope to ensure personalised guidelines can be adopted as soon as possible by doctors throughout Europe and America. Dr Sonya Babu-Narayan, Clinical Director at the British Heart Foundation and clinical cardiologist, said: "Hypertrophic cardiomyopathy is a severe, potentially life-threatening condition, and missed diagnosis means people that might benefit from new and effective treatments could slip through the net. At the same time, a diagnosis is itself a life changing event and we should be making every effort to prevent misdiagnosing people. "By updating the traditional one-size-fits-all approach, this study redefines abnormal heart wall thickness, a key contributor to the diagnosis of hypertrophic cardiomyopathy. As a result, more women and small individuals were identified who would otherwise be underdiagnosed. "Whilst other diagnostic factors are also important, this more personalised approach to defining abnormal heart muscle thickness heralds a new era for accurate diagnosis for patients and families affected by hypertrophic cardiomyopathy."
[2]
New study highlights gender differences in diagnosing heart condition
University College LondonJan 10 2025 Women may be missing a diagnosis of a potentially deadly heart condition due to guidelines that don't account for natural differences in sex and body size, according to a new study led by UCL (University College London) researchers. The research, published in the Journal of the American College of Cardiology and funded by the British Heart Foundation, details how current guidelines might be changed after showing a new personalised approach improves diagnosis accuracy. When they tested their updated approach in 1,600 patients with clinically diagnosed hypertrophic cardiomyopathy (HCM), the researchers found that it was particularly beneficial for women, increasing identification by 20 percentage points. The new method takes people's age, sex and size into account to determine whether their heart muscle is dangerously large. As well as preventing people being missed, it could also reduce the number of people mis-diagnosed with HCM. Around one in 500 people in the UK have HCM, a genetic condition where the muscular wall of the heart becomes thickened, making it harder for the heart to pump blood around the body. It can cause life-threatening problems like abnormal heart rhythms, which can lead to cardiac arrest and sudden death. Typically, two-thirds of people currently diagnosed with HCM are men, but researchers say women are just as likely to have the condition. There is no single gold standard test used to diagnose HCM. Doctors review a variety of tests and scan results. The most important of these involves measuring the thickness of the wall of the left ventricle, the heart's main pumping chamber. For 50 years the threshold for diagnosing HCM this way has been 15 millimetres for everyone - if the muscle is thicker than this, a patient is considered likely to have HCM. Dr. Hunain Shiwani (UCL Institute of Cardiovascular Science and St Bartholomew's Hospital), who led the research, said: "It is clear that this threshold, which is based on the results of studies from the 1970s, needs to be reconsidered. Having the same cut off for everyone regardless of age, sex or size completely ignores the fact that heart wall thickness is strongly influenced by these factors. "Our research provides a long-overdue update, showing that a personalized approach improves the accuracy of diagnosis. Effective treatments for HCM are starting to be used for the first time, making it more important than ever that we can correctly identify those who need them." The team used an AI tool they developed to analyze MRI heart scans with greater precision and in much less time than a human can. The tool was given 5,000 MRI scans of healthy hearts and measured the thickness of the left ventricle wall in each. From these data, the researchers were able to determine what normal ventricle wall thickness is for people of different ages, sexes, and sizes - measured by body surface area. This allowed them to set thresholds for abnormal wall thickness, indicating HCM, depending on a person's age, sex and size. The threshold was set higher if the person was older, larger or a man, and lower if they were younger, smaller or a woman. After testing the accuracy of the new thresholds in the group of HCM patients, the researchers applied them, as well as the current 15 mm cut-off, to a group of over 43,000 participants in the UK Biobank. For every eight people identified with possible HCM using the current threshold, only one was a woman. People identified were also much taller, heavier and older than the population average. When the new personalised thresholds were applied instead, the overall number of people identified was lower, suggesting fewer misdiagnoses. Importantly, there was a much more even split between men and women - with women making up 44% of those identified - a much more realistic finding since HCM should affect men and women equally. By incorporating other key factors, including ethnicity, and ensuring the new thresholds work with echocardiogram scans, which are more commonly used clinically, the team hope to ensure personalised guidelines can be adopted as soon as possible by doctors throughout Europe and America. Dr. Sonya Babu-Narayan, Clinical Director at the British Heart Foundation and clinical cardiologist, said: "Hypertrophic cardiomyopathy is a severe, potentially life-threatening condition, and missed diagnosis means people that might benefit from new and effective treatments could slip through the net. At the same time, a diagnosis is itself a life changing event and we should be making every effort to prevent misdiagnosing people. "By updating the traditional one-size-fits-all approach, this study redefines abnormal heart wall thickness, a key contributor to the diagnosis of hypertrophic cardiomyopathy. As a result, more women and small individuals were identified who would otherwise be underdiagnosed. "Whilst other diagnostic factors are also important, this more personalized approach to defining abnormal heart muscle thickness heralds a new era for accurate diagnosis for patients and families affected by hypertrophic cardiomyopathy." University College London
[3]
AI tool uncovers gender disparity in heart disease diagnosis
Women may be missing a diagnosis of a potentially deadly heart condition due to guidelines that don't account for natural differences in sex and body size, according to a new study led by UCL researchers. The research, published in the Journal of the American College of Cardiology, details how current guidelines might be changed after showing a new personalized approach improves diagnosis accuracy. When they tested their updated approach in 1,600 patients with clinically diagnosed hypertrophic cardiomyopathy (HCM), the researchers found that it was particularly beneficial for women, increasing identification by 20 percentage points. The new method takes people's age, sex and size into account to determine whether their heart muscle is dangerously large. As well as preventing people being missed, it could also reduce the number of people mis-diagnosed with HCM. Around one in 500 people in the UK have HCM, a genetic condition where the muscular wall of the heart becomes thickened, making it harder for the heart to pump blood around the body. It can cause life-threatening problems like abnormal heart rhythms, which can lead to cardiac arrest and sudden death. Typically, two-thirds of people currently diagnosed with HCM are men, but researchers say women are just as likely to have the condition. There is no single gold standard test used to diagnose HCM. Doctors review a variety of tests and scan results. The most important of these involves measuring the thickness of the wall of the left ventricle, the heart's main pumping chamber. For 50 years, the threshold for diagnosing HCM this way has been 15 millimeters for everyone -- if the muscle is thicker than this, a patient is considered likely to have HCM. Dr. Hunain Shiwani (UCL Institute of Cardiovascular Science and St Bartholomew's Hospital), who led the research, said, "It is clear that this threshold, which is based on the results of studies from the 1970s, needs to be reconsidered. Having the same cut off for everyone regardless of age, sex or size completely ignores the fact that heart wall thickness is strongly influenced by these factors. "Our research provides a long-overdue update, showing that a personalized approach improves the accuracy of diagnosis. Effective treatments for HCM are starting to be used for the first time, making it more important than ever that we can correctly identify those who need them." The team used an AI tool they developed to analyze MRI heart scans with greater precision and in much less time than a human can. The tool was given 5,000 MRI scans of healthy hearts and measured the thickness of the left ventricle wall in each. From these data, the researchers were able to determine what normal ventricle wall thickness is for people of different ages, sexes, and sizes -- measured by body surface area. This allowed them to set thresholds for abnormal wall thickness, indicating HCM, depending on a person's age, sex and size. The threshold was set higher if the person was older, larger or a man, and lower if they were younger, smaller or a woman. After testing the accuracy of the new thresholds in the group of HCM patients, the researchers applied them, as well as the current 15 mm cut-off, to a group of over 43,000 participants in the UK Biobank. For every eight people identified with possible HCM using the current threshold, only one was a woman. People identified were also much taller, heavier and older than the population average. When the new personalized thresholds were applied instead, the overall number of people identified was lower, suggesting fewer misdiagnoses. Importantly, there was a much more even split between men and women -- with women making up 44% of those identified -- a much more realistic finding since HCM should affect men and women equally. By incorporating other key factors, including ethnicity, and ensuring the new thresholds work with echocardiogram scans, which are more commonly used clinically, the team hope to ensure personalized guidelines can be adopted as soon as possible by doctors throughout Europe and America. Dr. Sonya Babu-Narayan, Clinical Director at the British Heart Foundation and clinical cardiologist, said, "Hypertrophic cardiomyopathy is a severe, potentially life-threatening condition, and missed diagnosis means people that might benefit from new and effective treatments could slip through the net. At the same time, a diagnosis is itself a life changing event and we should be making every effort to prevent misdiagnosing people. "By updating the traditional one-size-fits-all approach, this study redefines abnormal heart wall thickness, a key contributor to the diagnosis of hypertrophic cardiomyopathy. As a result, more women and small individuals were identified who would otherwise be underdiagnosed. "While other diagnostic factors are also important, this more personalized approach to defining abnormal heart muscle thickness heralds a new era for accurate diagnosis for patients and families affected by hypertrophic cardiomyopathy."
[4]
Outdated guidelines mean doctors failing to spot heart condition in women
Research finds hypertrophic cardiomyopathy testing that overlooks sex differences and body size is inadequate Doctors are failing to diagnose women with a potentially deadly heart condition because tests rely on outdated studies from the 1970s and do not account for natural differences in sex and body size. Hypertrophic cardiomyopathy (HCM) is a genetic condition where the muscular wall of the heart becomes thickened, making it harder for the heart to pump blood around the body. It affects one in 500 people, and can cause cardiac arrest and sudden death. But research funded by the British Heart Foundation found current guidelines for diagnosing the condition were wholly inadequate. The findings were published in the Journal of the American College of Cardiology. Two in three people diagnosed with HCM are men, but researchers said women were just as likely to have the condition. HCM is diagnosed using a variety of tests and scans, such as measuring the thickness of the wall of the left ventricle, the heart's main pumping chamber. For the past five decades, the threshold for diagnosing HCM has been 15mm for everyone. If the muscle is thicker than this, the patient is considered likely to have HCM. Research found this was inadequate and did not account for natural differences in sex and body size. The study included 1,600 patients with HCM whose condition was examined using a new method, taking account of age, sex and size. Researchers found that the new method, which included AI reading thousands of heart scans, was particularly beneficial for women, increasing identification of HCM by 20 percentage points. Further testing was carried out on data from more than 43,000 people on the UK Biobank. When the new personalised thresholds were applied, the overall number of people identified with HCM was lower, suggesting fewer misdiagnoses. There was also a more even split between men and women, with women making up 44% of those identified, reflecting the belief that women have been missing out on diagnosis. Dr Hunain Shiwani, a clinical research fellow at University College London and St Bartholomew's hospital, who led the research, said the current threshold was based on studies from the 1970s and needed to be reconsidered. He said: "Having the same cut-off for everyone regardless of age, sex or size completely ignores the fact that heart wall thickness is strongly influenced by these factors. "Our research provides a long-overdue update showing that a personalised approach improves the accuracy of diagnosis. "Effective treatments for HCM are starting to be used for the first time, making it more important than ever that we can correctly identify those who need them." Dr Sonya Babu-Narayan, a clinical director at the British Heart Foundation and a clinical cardiologist, said: "Hypertrophic cardiomyopathy is a severe, potentially life-threatening condition, and missed diagnosis means people that might benefit from new and effective treatments could slip through the net. "At the same time, a diagnosis is itself a life-changing event and we should be making every effort to prevent misdiagnosing people. "By updating the traditional one-size-fits-all approach, this study redefines abnormal heart wall thickness, a key contributor to the diagnosis of hypertrophic cardiomyopathy. "As a result, more women and small individuals were identified who would otherwise be underdiagnosed."
Share
Share
Copy Link
A new study led by UCL researchers reveals that current guidelines for diagnosing hypertrophic cardiomyopathy (HCM) may be missing cases in women due to outdated, one-size-fits-all criteria. An AI-powered personalized approach shows promise in improving diagnostic accuracy.

Outdated Guidelines Lead to Underdiagnosis of Heart Condition in Women
A groundbreaking study led by researchers at University College London (UCL) has revealed that current guidelines for diagnosing hypertrophic cardiomyopathy (HCM) may be failing to identify the condition in women due to outdated criteria that don't account for natural differences in sex and body size
1
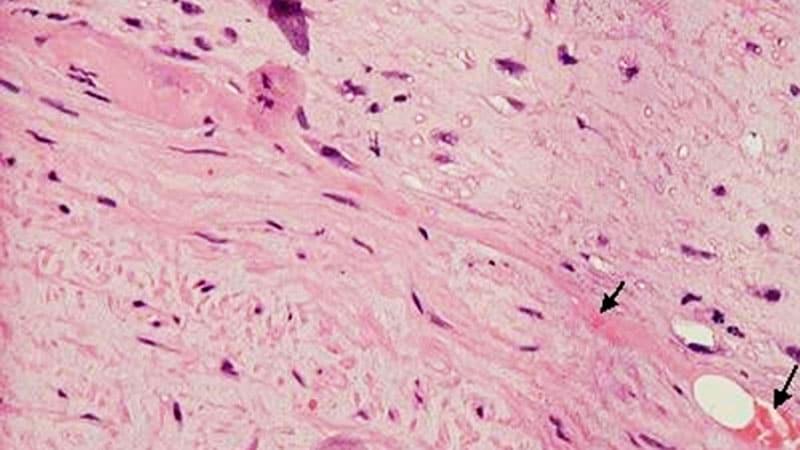
.Understanding Hypertrophic Cardiomyopathy
HCM is a genetic condition affecting approximately one in 500 people in the UK. It causes the muscular wall of the heart to thicken, making it harder for the heart to pump blood effectively. This can lead to life-threatening complications such as abnormal heart rhythms, cardiac arrest, and sudden death
2
.The Problem with Current Diagnostic Methods
For the past 50 years, the threshold for diagnosing HCM has been a left ventricle wall thickness of 15 millimeters for all patients, regardless of age, sex, or body size. This one-size-fits-all approach, based on studies from the 1970s, has led to a significant disparity in diagnoses between men and women
3
.AI-Powered Personalized Approach
The research team developed an AI tool to analyze MRI heart scans with greater precision and speed than human capabilities. By examining 5,000 MRI scans of healthy hearts, they determined normal ventricle wall thickness for people of different ages, sexes, and sizes
1
.This data allowed them to establish personalized thresholds for abnormal wall thickness, taking into account an individual's age, sex, and body surface area. The new method sets higher thresholds for older, larger individuals and men, while lower thresholds are applied to younger, smaller individuals and women
2
.Improved Diagnostic Accuracy
When tested on 1,600 patients with clinically diagnosed HCM, the new approach showed particular benefits for women, increasing identification by 20 percentage points. Further testing on over 43,000 UK Biobank participants revealed a more balanced distribution between men and women, with women comprising 44% of those identified – a more realistic representation of HCM's equal prevalence across sexes
3
.Related Stories
Implications for Future Diagnoses
Dr. Hunain Shiwani, who led the research, emphasized the importance of this update: "Our research provides a long-overdue update, showing that a personalized approach improves the accuracy of diagnosis. Effective treatments for HCM are starting to be used for the first time, making it more important than ever that we can correctly identify those who need them"
4
.Next Steps
The research team aims to incorporate additional factors such as ethnicity and ensure the new thresholds work with echocardiogram scans, which are more commonly used in clinical settings. Their goal is to implement these personalized guidelines in Europe and America as soon as possible, ushering in a new era of accurate diagnosis for patients and families affected by hypertrophic cardiomyopathy
1
.References
Summarized by
Navi
[1]
[3]
Related Stories
AI Model Identifies Female Patients at Higher Risk of Heart Disease Using ECG Analysis
26 Feb 2025•Health

AI Revolutionizes Heart Disease Detection: From ECGs to Hidden Conditions
17 Jul 2025•Health
Mount Sinai Researchers Enhance AI Algorithm to Improve Detection and Risk Assessment of Hypertrophic Cardiomyopathy
23 Apr 2025•Health
Recent Highlights
1
SpaceX acquires xAI in $1.25 trillion merger, plans 1 million satellite data centers in orbit
Business and Economy

2
EU launches formal investigation into Grok over sexualized deepfakes and child abuse material
Policy and Regulation

3
SpaceX files to launch 1 million satellites as orbital data centers for AI computing power
Technology





