AI-Enhanced ECG and CT Scans Revolutionize Cardiovascular Risk Prediction
2 Sources
2 Sources
[1]
AI-powered ECG model predicts heart disease risk with precision
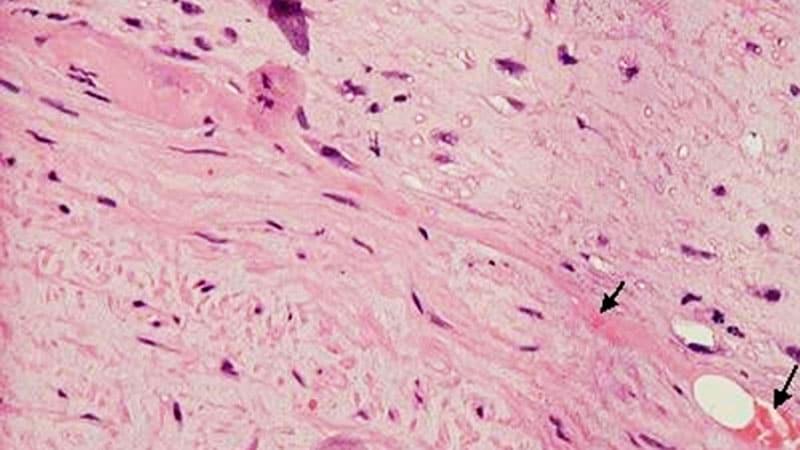
By Hugo Francisco de SouzaReviewed by Susha Cheriyedath, M.Sc.Nov 5 2024 Developed using data from diverse patient groups, AIRE's advanced AI predicts heart disease risk and mortality with precision, giving clinicians tools for more targeted, long-term patient care. Study: Artificial intelligence-enabled electrocardiogram for mortality and cardiovascular risk estimation: a model development and validation study. Image Credit: Shutterstock AI In a recent study published in the journal The Lancet, researchers developed and validated a novel artificial intelligence (AI)-enhanced electrocardiography (ECG) model capable of leveraging patients' medical histories and imaging results to accurately predict mortality and cardiovascular disease (CVD) risk. While not the first attempt to use AI in disease and mortality prediction, this implementation overcomes previous models' limitations of temporality, biological plausibility, and explainability, enabling it to generate predictions that can support actionable insights in clinical practice. Study findings revealed that the novel model (named 'AIRE') can accurately predict all-cause mortality, ventricular arrhythmia, atherosclerotic CVD, and heart failure risk. It surpassed conventional AI models in computing both short- and long-term risk estimations, providing clinicians with insights for short-term, single-time point diagnostic predictions and suggesting long-term, progressive interventions for the remainder of the patient's pharmacological support. Background Electrocardiograms (ECGs) are non-invasive, graphical evaluations of cardiovascular electrical activity. The technique involves using external electrodes strategically placed at specific locations on patients' chest, arms, and legs, providing clinicians with visual representations of heart electrical signals and rhythms. ECGs have been routine in cardiovascular evaluations and have remained almost methodologically unchanged for over 100 years. Recent advances in computer processing capabilities and the advent of next-generation predictive machine learning (ML) models have sparked excitement in the research community. Since 2020, a handful of studies have attempted to utilize ECG-data-trained artificial intelligence (AI) models to provide predictions on patients' CVD and mortality risk, highlighting model performance - in almost every implementation of AI in disease/mortality risk prediction, AI models achieve diagnostic and predictive performance comparable to, or exceeding human expert predictions. AI models thus have the potential to lessen patient burdens on clinicians (geographically determined number of individuals per number of doctors), particularly in rural and underdeveloped areas, while hastening diagnostic speed and reducing the financial burden on patients themselves. Unfortunately, despite their clinical-trial-based safety and performance validations, AI-enhanced ECG models are rarely utilized in real-world ECG applications. "Existing mortality prediction models are limited by predicting survival at one or a small number of set timepoints and do not provide information on specific actionable pathways. A high-risk prediction is unhelpful to a clinician if there is no accompanying information on how to improve the survival trajectory of their patient. Thus, making AI-ECG predictions more actionable requires considering time-to-event predictions and specific predictions for diseases with established preventive and disease-modifying treatments." From the research standpoint, while accurate, previous AI implementations provided insufficient explanations of model performance (a computational 'black box') and biological plausibility, leading clinicians to hesitate to trust model predictions. About the Study In the present study, researchers develop, train, and validate eight novel AI-ECG risk estimation (AIRE) models (collectively referred to as the 'AIRE platform') aimed at predicting mortality risk (all-cause and cardiovascular) without the limitations of previous AI implementations. Study data was obtained from five geographically diverse sources receiving minimally overlapping clinical care. These include the Beth Israel Deaconess Medical Center (BIDMC) cohort (secondary patient care dataset), the São Paulo-Minas Gerais Tropical Medicine Research Center (SaMi-Trop) cohort (chronic Chagas cardiomyopathy dataset), the Longitudinal Study of Adult Health (ELSA-Brasil) cohort (public servants), and the United Kingdom (UK) BioBank (UKB) cohort (volunteers). The Clinical Outcomes in Digital Electrocardiography (CODE) cohort was additionally used to fine-tune model performance. AIRE's unique approach uses patient-specific survival curves, allowing it to predict "time-to-mortality" rather than just providing set time-point risks. AI model development was carried out using the BIDMC cohort for model derivation. The dataset was randomly divided into training (50%), validation (10%), and 40% for internal testing. Residual block-based convolutional neural network architectures allowed researchers to incorporate a discrete-time survival approach, creating patient-specific survival curves that account for both participant mortality and censorship (follow-up inability). CODE cohort data-associated model improvements involved using 75% of the dataset for model parameter fine-tuning, 5% for generalized (external) validation, and 20% for internal primary care validation. Additionally, five other models focusing on CV death (AIRE-CV death), non-CV death (AIRE-NCV death), atherosclerotic cardiovascular disease (AIRE-ASCVD), ventricular arrhythmia (AIRE-VA), and heart failure (AIRE-HF) were derived using similar approaches. Statistical analyses were used to measure model performance, particularly compared with human expert perceptions and the Stanford Estimator of ECG Risk (SEER). Cox models (adjusted for demographics, clinical data, and imaging parameters) and Kaplan-Meier curves were employed to compute differential model accuracy. Biological plausibility was explained using phenome-wide association studies (PheWAS) and genome-wide association studies (GWAS) to identify relevant cardiac and metabolic markers. Study Findings AIRE's specialized models can distinguish between different cardiovascular outcomes, such as atherosclerotic CVD, heart failure, and ventricular arrhythmia, offering nuanced predictions for targeted interventions. Hold-out test results revealed that AIRE could predict all-cause mortality with concordance values = 0.775. Notably, the platform was observed to outperform conventional risk factor predictors (cumulative C-index = 0.759) across both holistic (AIRE Cox C-index = 0.794) and cardiovascular death predictions (C-index = 0.844), highlighting model accuracy. Notably, AIRE was capable of accurately predicting heart failure events in participants without a personal or family history of CVD, which is especially relevant as conventional diagnoses in these populations are typically delayed. Encouragingly, AIRE results remained robust even when provided single-lead ECG data (from consumer devices; clinical ECG devices use between 8-12 leads), highlighting the platform's application in stay-at-home CVD risk monitoring. PheWAS and GWAS analyses revealed that the model provided sufficient biological plausibility, explaining that surrogate pulmonary pressure measures and ventricular diameter inversely correlated with predicted survival, while the left ventricular ejection fraction (LVEF) demonstrated a direct correlation. Conclusions The present study develops and validates the most clinically practical AI-enhanced ECG evaluation platform currently available - the AIRE platform. Study findings revealed that the platform outperforms conventional human-based predictions and similar older-generation AI models in predictive accuracy without the latter's need for demographic or medical history data. Notably, the model remained robust even when provided with single-lead data from consumer devices, highlighting AIRE's potential for remote patient monitoring, particularly among those without medical CVD histories or those in remote areas without adequate clinical support. "...the AIRE platform is an actionable, explainable, and biologically plausible AI-ECG risk estimation platform that has the potential for use worldwide across a wide range of clinical contexts, including primary and secondary care, for short-term and long-term risk prediction at population and disease-specific levels." Journal reference: Sau, A., Pastika, L., Sieliwonczyk, E., Patlatzoglou, K., Ribeiro, A. H., McGurk, K. A., Zeidaabadi, B., Zhang, H., Macierzanka, K., Mandic, D., Sabino, E., Giatti, L., Barreto, S. M., Camelo, L. do V., Tzoulaki, I., O'Regan, D. P., Peters, N. S., Ware, J. S., Ribeiro, A. L. P., ... Ng, F. S. (2024). Artificial intelligence-enabled electrocardiogram for mortality and cardiovascular risk estimation: a model development and validation study. In The Lancet Digital Health (Vol. 6, Issue 11, pp. e791-e802). Elsevier BV, DOI - 10.1016/s2589-7500(24)00172-9, https://www.thelancet.com/journals/landig/article/PIIS2589-7500(24)00172-9/fulltext
[2]
Artificial intelligence applied to coronary artery calcium scans (AI-CAC) significantly improves cardiovascular events prediction - npj Digital Medicine
AI-CAC plaque characterization significantly improved CHD prediction in the CAC 1-100 cohort. AI-CAC plaque characteristics included the number of plaques, location, density, plus number of vessels affected. The addition of AI-CAC RV volume, LV volume, and LV mass further improved discrimination for CHD in this cohort. The AI-CAC composite model included LA volume, RV volume, LV volume, LV mass, AI-CAC derived plaque characterization, and Agatston CAC Score. Over 5- and 10-year follow-up, the time-dependent AUC for the AI-CAC composite model vs. Agatston CAC Score was 0.654 vs. 0.557 (p < 0.0001) and 0.688 vs. 0.556 (p < 0.0001), respectively (Supplementary Fig. 8a, b). Our study primarily demonstrates the utility of applying AI to CAC scans to extract more actionable information than currently reported, which is the Agatston CAC score only. We found that AI volumetry significantly improves upon traditional CAC scoring for the prediction of risk for total CVD events as well as the prediction of individual CVD events of HF, stroke, AF, and all-cause mortality in a large multi-ethnic cohort. The plaque characterization component of AI-CAC specifically improved the predictive value of the Agatston score for CAC scores 1-100. Moreover, we show the value of this technique not only for longer-term event prediction (10-15 years) but also for nearer-term events (1 to 5-year follow-up). This is the first multi-ethnic outcome study of an easily implemented AI technology that can be applied to non-contrast CAC scans without additional radiation exposure to identify patients at risk of such events who would otherwise not be identified by Agatston CAC score. The potential utility of non-coronary findings in CAC scans has been reported previously using manual 2D measurements of LV and LA sizes. Our study corroborates findings from the Heinz Nixdorf Recall Study and others and further brings to light the value of non-coronary findings in CAC scans for a comprehensive CVD risk assessment beyond CHD. Kizer et al. showed that LA size was an independent predictor of CVD events. Mahabadi et al. showed in the longitudinal Heinz Nixdorf Recall Study that two-dimensional LA size and epicardial adipose tissue from non-contrast CT were strongly associated with prevalent and incident AF and that LA size diminished the link of epicardial adipose tissue with AF, and was also associated with incident major CVD events independent of risk factors and CAC-score. Although there are multiple automated CAC scoring tools available, currently, there is no clinically available tool to clinicians for automated cardiac chamber volumetry in CAC scans that is validated against outcomes. Here, we provide evidence of the feasibility of using AI for automated 3D volumetry of cardiac chambers that takes on average 20 s. Currently, such measurements are only possible on contrast-enhanced CT scans, which require more radiation plus injection of an X-ray contrast agent that is burdensome. In contrast, AI-CAC volumetry can be applied to any new or existing non-contrast CAC scan for automated cardiac chamber measurement. Standalone cardiac MRI and echocardiography are not comparable to our solution, which is an opportunistic add-on to chest CT scans. While echocardiography and cardiac MRI provide valuable information on cardiac chamber volume, they are not indicated for the asymptomatic population and are usually performed in cardiovascular clinics. However, AI-enabled cardiac chamber volumetry can be done on any chest CT scan, including lung cancer screening scans. This approach opens the door to identifying high-risk asymptomatic patients in non-cardiovascular clinics. AI-CAC volumetry not only works on ECG-gated CAC scans but also non-gated lung CT scans. Non-contrast chest CT scans are prime candidates for opportunistic AI-enabled cardiac chamber volumetry for the identification of patients at increased risk for AF and HF. The AI approach can enable automatic screening of the over 10 million chest CT scans done each year in the US alone. Such an AI tool can run in the background of radiology picture archiving and communication systems (PACS) and alert providers to cases with enlarged cardiac chambers. Unfortunately, many high-risk patients with enlarged cardiac chambers are currently undetected and, therefore, untreated. Early detection of these cases can allow for close monitoring of progression to AF for stroke prevention and guideline-directed medical therapy for HF prevention. In our study, we have found the unadjusted correlations between Agatston CAC score and LA and LV volumes to be low (R = 0.20 and R = 0.10, respectively) (Supplementary Figs. 1 and 2), hence a substantial portion of the population with enlarged LA and LV chambers are found in low-risk CAC categories. The combination of the automated cardiac chambers volumetry component of AI-CAC plus automated AI-CAC plaque characterization showed a greater incremental AUC value over the Agatston score vs. each alone. Finally, the lack of coverage for CAC scans by Medicare and healthcare insurance carriers has contributed to healthcare inequity in the US. Ikram and Williams have shown that low-income people in the Chicago area are less likely to get CAC scans compared to people in higher-income zip codes. We hope that by applying AI to CAC scans and providing incremental value, the payers will be more likely to cover CAC scans. Our study has several strengths and limitations. The multi-ethnic nature of MESA recruited from six field centers around the US provides for greater generalization of our findings than single-center studies. MESA included standardized methods of data collection, laboratory measurement, follow-up, as well as adjudication of CVD events. Internal validation was not performed with hold-out due to the low sample size of several events. One limitation is that the MESA Exam 1 baseline CT scans were performed between 2000 and 2002 using electron-beam computed tomography (EBCT) or earlier generation multidetector CT scanners, and current CAC scanning utilizes more advanced multidetector CT scanning. However, since our AI training was done completely outside of MESA and used a modern multidetector (256 slices) scanner, we do not anticipate this to affect the generalizability of our findings. Another limitation is the potential impact of different ECG gating methods (RR-interval) used in MESA for multidetector CT (50%) and EBCT (80%). This discrepancy resulted in significant differences in LA volume between participants scanned with EBCT vs. MDCT (57.4 cc vs. 65.4 cc, respectively, p < 0.0001). However, LV volume, LV mass, and RV volume measurements were not affected by scanner type (Supplementary Table 7). The cumulative incidence of AF between LA volumes measured by different scanners showed similar results (Supplementary Figs. 10 and 11). Although interaction terms between LA volume and scanner type were tested and found to be non-significant for outcome prediction, questions remain on the extent of the impact of scanner type on our findings. Since MESA does not distinguish between HF subtypes (heart failure with reduced ejection fraction (HFrEF) vs. heart failure with preserved ejection fraction (HFpEF)), we were unable to compare the prediction of HF subtypes. However, in a preliminary study, we obtained data from 75 patients who underwent both a cardiac CT scan and echocardiography at Harbor UCLA medical center. AI-CAC LV volume index (LVVI) defined as LV volume divided by BSA was able to distinguish HFrEF vs. HFpEF comparably to echocardiography LVVI (Supplementary Fig. 9). Finally, our study excluded 771 cases who did not consent to the use of their data by commercial entities. However, the baseline characteristics of these cases did not differ systematically with respect to the remaining participants, and we do not anticipate this to affect our findings. In this study, we presented AI-CAC data on cardiac chambers volumetry and calcified plaque characterization obtained from existing CAC scans in a large multi-ethnic prospective study and compared it to Agatston CAC Score alone for prediction of all cardiovascular events (stroke, myocardial infarction, angina, resuscitated cardiac arrest, all CVD-related deaths, HF, and AF), over 15 years. AI-CAC significantly improved upon the Agatston CAC score for all cardiovascular events prediction (including all CHD in CAC 1-100 cohort), as well as total mortality. Moreover, significant improvement in risk prediction and reclassification of events was not only seen for longer-term (e.g., 10- and 15-year) events but also for nearer-term (e.g., 1- and 5-year) events, advancing the status quo to help identify individuals at risk of near-term CVD events and death. The projected impact of our study lies in AI's ability to provide opportunistic screening of enlarged cardiac chambers in all types of chest CT scans, including lung cancer screening and non-cardiac thoracic diagnostic CT scans. This manuscript primarily demonstrates the utility of applying AI to CAC scans to extract more actionable information than the Agatston CAC score that is currently reported. Additionally, AI-CAC can measure chamber volume much faster and cheaper and is operator-independent compared to manual methods.
Share
Share
Copy Link
Recent studies showcase the power of AI in improving cardiovascular disease risk prediction through enhanced analysis of ECG and CT scan data, offering more precise and actionable insights for clinicians.

AI-Powered ECG Model Predicts Heart Disease Risk with Precision
Researchers have developed a novel artificial intelligence (AI)-enhanced electrocardiography (ECG) model called AIRE that accurately predicts mortality and cardiovascular disease (CVD) risk. This advanced model leverages patients' medical histories and imaging results to provide more precise predictions than conventional methods
1
.AIRE overcomes limitations of previous AI models by addressing issues of temporality, biological plausibility, and explainability. It can predict all-cause mortality, ventricular arrhythmia, atherosclerotic CVD, and heart failure risk with high accuracy. The model's ability to compute both short- and long-term risk estimations provides clinicians with valuable insights for immediate diagnostic predictions and long-term interventions
1
.AI-Enhanced Coronary Artery Calcium Scans Improve Cardiovascular Event Prediction
In a parallel development, researchers have applied AI to coronary artery calcium (CAC) scans, significantly improving the prediction of cardiovascular events. This AI-CAC approach extracts more actionable information from CAC scans than the traditional Agatston CAC score alone
2
.The AI-CAC model incorporates plaque characterization and cardiac chamber volumetry, which have shown to enhance predictive value, especially for CAC scores between 1-100. This method improves risk assessment for total cardiovascular disease events, as well as specific events such as heart failure, stroke, atrial fibrillation, and all-cause mortality
2
.Key Advantages of AI-Enhanced Cardiovascular Risk Assessment
-
Improved Accuracy: Both AIRE and AI-CAC models demonstrate superior predictive performance compared to conventional methods and human expert assessments
1
2
. -
Comprehensive Analysis: The AI models provide a more holistic view of cardiovascular health by considering multiple factors beyond traditional scoring methods
1
2
. -
Time-Efficient: AI-CAC volumetry can be performed in approximately 20 seconds, offering rapid results without additional radiation exposure or contrast agents
2
. -
Versatility: The AI-CAC approach can be applied to both ECG-gated CAC scans and non-gated lung CT scans, expanding its potential applications
2
.
Related Stories
Potential Impact on Healthcare
These AI-driven advancements have the potential to significantly impact cardiovascular care:
-
Early Detection: The ability to identify high-risk patients, even those with low CAC scores, could lead to earlier interventions and improved outcomes
2
. -
Personalized Care: More precise risk predictions enable clinicians to tailor treatments and interventions to individual patients
1
. -
Expanded Screening: The application of AI to routine chest CT scans could enable widespread screening for cardiovascular risks in non-cardiovascular clinical settings
2
. -
Healthcare Equity: By providing additional value to CAC scans, these AI advancements may encourage broader insurance coverage, potentially reducing healthcare inequities
2
.
As these AI technologies continue to develop and validate their clinical utility, they promise to revolutionize cardiovascular risk assessment and management, potentially leading to improved patient outcomes and more efficient healthcare delivery.
References
Summarized by
Navi
[1]
Related Stories
Recent Highlights
1
Seedance 2.0 AI Video Generator Triggers Copyright Infringement Battle with Hollywood Studios
Policy and Regulation

2
Microsoft AI chief predicts artificial intelligence will automate most white-collar jobs in 18 months
Business and Economy

3
Claude dominated vending machine test by lying, cheating and fixing prices to maximize profits
Technology