AI-Guided Patient Stratification Revolutionizes Alzheimer's Drug Trials
2 Sources
2 Sources
[1]
AI-guided patient stratification boosts Alzheimer's trial outcomes and efficiency
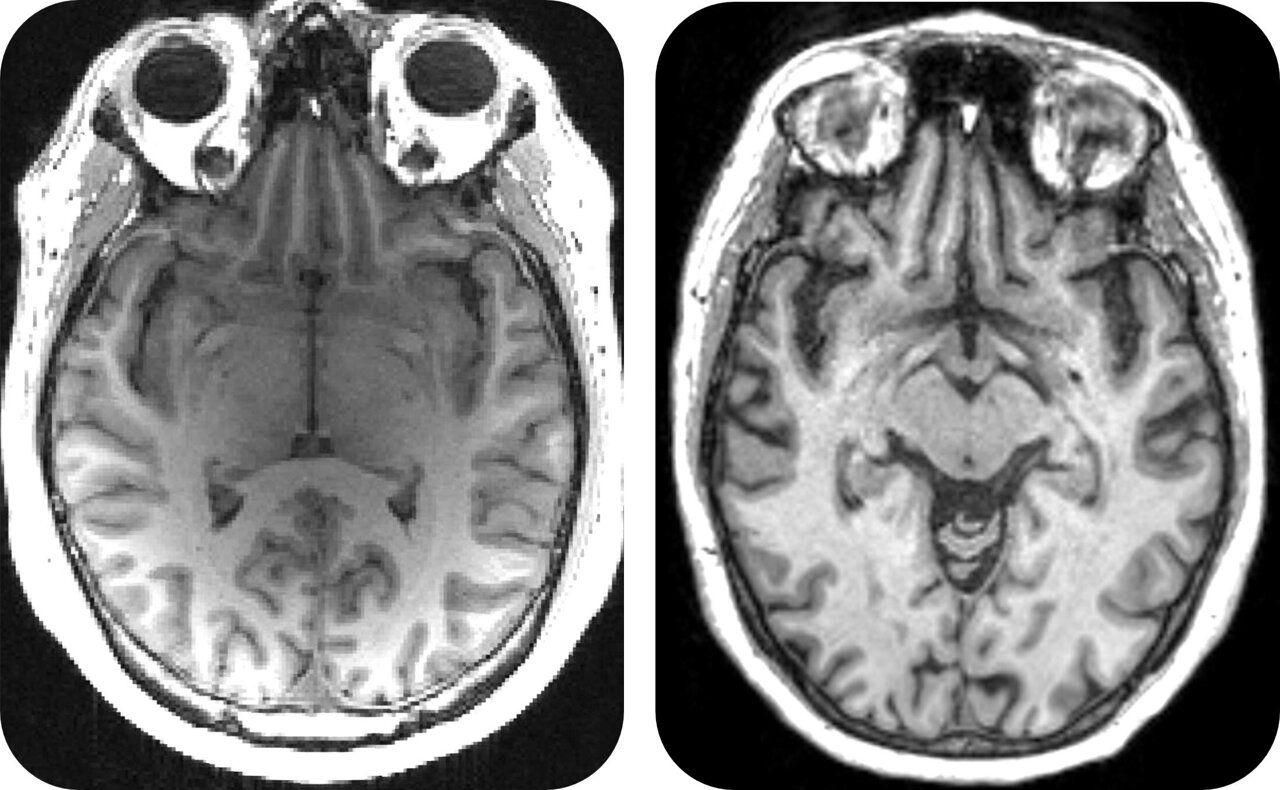
University of CambridgeJul 17 2025 Scientists have used an AI model to reassess the results of a completed clinical trial for an Alzheimer's disease drug. They found the drug slowed cognitive decline by 46% in a group of patients with early stage, slow-progressing mild cognitive impairment - a condition that can progress to Alzheimer's. Using AI allowed the team to split trial participants into two groups: either slowly or rapidly progressing towards Alzheimer's disease. They could then look at the effects of the drug on each group. More precise selection of trial participants in this way could help select patients most likely to benefit from treatment, with the potential to reduce the cost of developing new medicines by streamlining clinical trials. The AI model developed by researchers at the University of Cambridge predicts whether, and how quickly, people at early stages of cognitive decline will progress to full-blown Alzheimer's. It gives predictions for patients that are three times more accurate than standard clinical assessments based on memory tests, MRI scans and blood tests. Using this patient stratification model, data from a completed clinical trial - which did not demonstrate efficacy in the total population studied - was re-analysed. The researchers found that the drug cleared a protein called beta amyloid in both patient groups as intended - but only the early stage, slow-progressing patients showed changes in symptoms. Beta amyloid is one of the first disease markers to appear in the brain in Alzheimer's disease. The new findings have significant implications: using AI to separate patients into different groups, such as slow versus rapidly progressing towards Alzheimer's disease, allows scientists to better identify those who could benefit from a treatment approach - potentially accelerating the discovery of much-needed new Alzheimer's drugs. The results are published today in the journal Nature Communications. Promising new drugs fail when given to people too late, when they have no chance of benefiting from them. With our AI model we can finally identify patients precisely, and match the right patients to the right drugs. This makes trials more precise, so they can progress faster and cost less, turbocharging the search for a desperately-need precision medicine approach for dementia treatment." Professor Zoe Kourtzi in the University of Cambridge's Department of Psychology, senior author of the report She added: "Our AI model gives us a score to show how quickly each patient will progress towards Alzheimer's disease. This allowed us to precisely split the patients on the clinical trial into two groups - slow, and fast progressing, so we could look at the effects of the drug on each group." Health Innovation East England, the innovation arm of the NHS in the East of England, is now supporting Kourtzi to translate this AI-enabled approach into clinical care for the benefit of future patients. Joanna Dempsey, Principal Advisor at Health Innovation East England, said: "This AI-enabled approach could have a significant impact on easing NHS pressure and costs in dementia care by enabling more personalised drug development - identifying which patients are most likely to benefit from treatment, resulting in faster access to effective medicines and targeted support for people living with dementia." Drugs like this are not intended as cures for Alzheimer's disease. The aim is to reduce cognitive decline so that patients don't get worse. Dementia is the UK's leading cause of death, and a major cause of mortality globally. It costs $1.3 tr per year, and the number of cases are expected to treble by 2050. There is no cure, and patients and families face high uncertainty. Despite decades of research and development, clinical trials of treatments for dementia have been largely unsuccessful. The failure rate for new treatments is unreasonably high at over 95%, despite $43 bn having been spent on research and development. Progress has been hampered by the wide variation in symptoms, disease progression and responses to treatment among patients. Although new dementia drugs have recently been approved for use in the US, their risk of side effects and insufficient cost effectiveness have prevented healthcare adoption in the NHS. Understanding and accounting for the natural differences among individuals with a disease is crucial, so that treatments can be tailored to be most effective for each patient. Alzheimer's disease is complex, and although some drugs are available to treat it they don't work for everybody. "AI can guide us to the patients who will benefit from dementia medicines, by treating them at the stage when the drugs will make a difference, so we can finally start fighting back against these cruel diseases. Making clinical trials faster, cheaper and better, guided by AI has strong potential to accelerate discovery of new precise treatments for individual patients, reducing side effects and costs for healthcare services," said Kourtzi. She added: "Like many people, I have watched hopelessly as dementia stole a loved one from me. We've got to accelerate the development of dementia medicines. Over £40 billion has already been spent over thirty years of research and development - we can't wait another thirty years." University of Cambridge Journal reference: Vaghari, D., et al. (2025). AI-guided patient stratification improves outcomes and efficiency in the AMARANTH Alzheimer's Disease clinical trial. Nature Communications. doi.org/10.1038/s41467-025-61355-3.
[2]
AI can accelerate search for more effective Alzheimer's medicines by streamlining clinical trials
Scientists have used an AI model to reassess the results of a completed clinical trial for an Alzheimer's disease drug. They found that the drug slowed cognitive decline by 46% in a group of patients with early-stage, slow-progressing mild cognitive impairment -- a condition that can progress to Alzheimer's. Using AI allowed the team to split trial participants into two groups: either slowly or rapidly progressing towards Alzheimer's disease. They could then look at the effects of the drug on each group. The work appears in Nature Communications. More precise selection of trial participants in this way could help select patients most likely to benefit from treatment, with the potential to reduce the cost of developing new medicines by streamlining clinical trials. The AI model developed by researchers at the University of Cambridge predicts whether and how quickly people at early stages of cognitive decline will progress to full-blown Alzheimer's. It gives predictions for patients that are three times more accurate than standard clinical assessments based on memory tests, MRI scans and blood tests. Using this patient stratification model, data from a completed clinical trial -- which did not demonstrate efficacy in the total population studied -- was re-analyzed. The researchers found that the drug cleared a protein called beta amyloid in both patient groups as intended -- but only the early stage, slow-progressing patients showed changes in symptoms. Beta amyloid is one of the first disease markers to appear in the brain in Alzheimer's disease. The new findings have significant implications. Using AI to separate patients into different groups, such as slow versus rapidly progressing towards Alzheimer's disease, allows scientists to better identify those who could benefit from a treatment approach -- potentially accelerating the discovery of much-needed new Alzheimer's drugs. Professor Zoe Kourtzi in the University of Cambridge's Department of Psychology, senior author of the report, said, "Promising new drugs fail when given to people too late, when they have no chance of benefiting from them. With our AI model, we can finally identify patients precisely, and match the right patients to the right drugs. This makes trials more precise, so they can progress faster and cost less, turbocharging the search for a desperately-needed precision medicine approach for dementia treatment. "Our AI model gives us a score to show how quickly each patient will progress towards Alzheimer's disease. This allowed us to precisely split the patients in the clinical trial into two groups -- slow- and fast-progressing, so we could look at the effects of the drug on each group." Health Innovation East England, the innovation arm of the NHS in the East of England, is now supporting Kourtzi to translate this AI-enabled approach into clinical care for the benefit of future patients. Joanna Dempsey, Principal Advisor at Health Innovation East England, said, "This AI-enabled approach could have a significant impact on easing NHS pressure and costs in dementia care by enabling more personalized drug development -- identifying which patients are most likely to benefit from treatment, resulting in faster access to effective medicines and targeted support for people living with dementia." Drugs like this are not intended as cures for Alzheimer's disease. The aim is to reduce cognitive decline so that patients don't get worse. Dementia is the UK's leading cause of death, and a major cause of mortality globally. It costs $1.3 trillion per year, and the number of cases is expected to triple by 2050. There is no cure, and patients and families face great uncertainty. Despite decades of research and development, clinical trials of treatments for dementia have been largely unsuccessful. The failure rate for new treatments is unreasonably high at over 95%, despite $43 billion having been spent on research and development. Progress has been hampered by the wide variation in symptoms, disease progression and responses to treatment among patients. Although new dementia drugs have recently been approved for use in the US, their risk of side effects and insufficient cost-effectiveness have prevented health care adoption in the NHS. Understanding and accounting for the natural differences among individuals with a disease is crucial, so that treatments can be tailored to be most effective for each patient. Alzheimer's disease is complex, and although some drugs are available to treat it, they don't work for everybody. "AI can guide us to the patients who will benefit from dementia medicines, by treating them at the stage when the drugs will make a difference, so we can finally start fighting back against these cruel diseases. Making clinical trials faster, cheaper and better, guided by AI, has strong potential to accelerate the discovery of new precise treatments for individual patients, reducing side effects and costs for health care services," said Kourtzi. She added, "Like many people, I have watched hopelessly as dementia stole a loved one from me. We've got to accelerate the development of dementia medicines. Over £40 billion has already been spent over thirty years of research and development -- we can't wait another thirty years."
Share
Share
Copy Link
Researchers at the University of Cambridge have developed an AI model that significantly improves the efficiency and outcomes of Alzheimer's drug trials by accurately predicting disease progression and stratifying patients.
AI Model Revolutionizes Alzheimer's Drug Trials
Researchers at the University of Cambridge have developed a groundbreaking AI model that could transform the landscape of Alzheimer's disease drug trials. The model, which predicts disease progression with unprecedented accuracy, has demonstrated its potential to significantly improve trial outcomes and efficiency
1
.Improved Patient Stratification
Source: News-Medical
The AI model's key innovation lies in its ability to stratify patients into slow-progressing and fast-progressing groups. This distinction allows researchers to more precisely evaluate drug efficacy in different patient populations. In a re-analysis of a completed clinical trial, the model revealed that the drug in question slowed cognitive decline by 46% in patients with early-stage, slow-progressing mild cognitive impairment
2
.Enhanced Prediction Accuracy
Professor Zoe Kourtzi, senior author of the study, emphasized the model's superior predictive power: "Our AI model gives us a score to show how quickly each patient will progress towards Alzheimer's disease. This allowed us to precisely split the patients on the clinical trial into two groups - slow, and fast progressing, so we could look at the effects of the drug on each group"
1
.The AI model's predictions are reportedly three times more accurate than standard clinical assessments based on memory tests, MRI scans, and blood tests
2
.
Source: Medical Xpress
Implications for Drug Development
This AI-guided approach has significant implications for the pharmaceutical industry and healthcare systems. By enabling more precise patient selection, it could potentially reduce the cost and time required for clinical trials, accelerating the development of new Alzheimer's treatments
1
.Joanna Dempsey from Health Innovation East England highlighted the potential impact: "This AI-enabled approach could have a significant impact on easing NHS pressure and costs in dementia care by enabling more personalised drug development - identifying which patients are most likely to benefit from treatment, resulting in faster access to effective medicines and targeted support for people living with dementia"
2
.Related Stories
Addressing the Alzheimer's Crisis
The development of this AI model comes at a critical time in Alzheimer's research. Despite decades of effort and billions spent on research and development, the failure rate for new treatments remains alarmingly high at over 95%
1
.Dementia, of which Alzheimer's is the most common form, is the UK's leading cause of death and a major global health concern. With cases expected to triple by 2050 and an annual cost of $1.3 trillion, the need for effective treatments is urgent
2
.Future Prospects
As the AI model transitions from research to clinical application, it holds the promise of ushering in a new era of precision medicine in Alzheimer's treatment. Professor Kourtzi concluded, "AI can guide us to the patients who will benefit from dementia medicines, by treating them at the stage when the drugs will make a difference, so we can finally start fighting back against these cruel diseases"
1
.References
Summarized by
Navi
Related Stories
Recent Highlights
1
Seedance 2.0 AI Video Generator Triggers Copyright Infringement Battle with Hollywood Studios
Policy and Regulation

2
Microsoft AI chief predicts artificial intelligence will automate most white-collar jobs in 18 months
Business and Economy

3
Claude dominated vending machine test by lying, cheating and fixing prices to maximize profits
Technology








