AI Model Outperforms Doctors in Predicting Sudden Cardiac Death Risk
4 Sources
4 Sources
[1]
AI spots deadly heart risk most doctors can't see
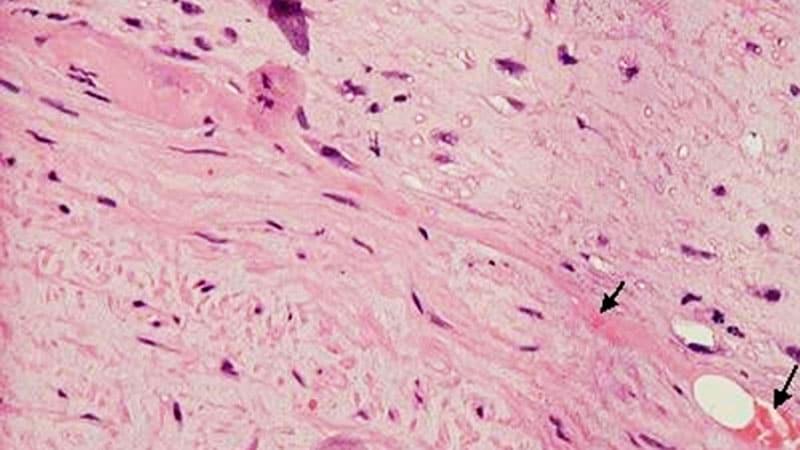
A new AI model is much better than doctors at identifying patients likely to experience cardiac arrest. The linchpin is the system's ability to analyze long-underused heart imaging, alongside a full spectrum of medical records, to reveal previously hidden information about a patient's heart health. The federally-funded work, led by Johns Hopkins University researchers, could save many lives and also spare many people unnecessary medical interventions, including the implantation of unneeded defibrillators. "Currently we have patients dying in the prime of their life because they aren't protected and others who are putting up with defibrillators for the rest of their lives with no benefit," said senior author Natalia Trayanova, a researcher focused on using artificial intelligence in cardiology. "We have the ability to predict with very high accuracy whether a patient is at very high risk for sudden cardiac death or not." The findings are published today in Nature Cardiovascular Research. Hypertrophic cardiomyopathy is one of the most common inherited heart diseases, affecting one in every 200 to 500 individuals worldwide, and is a leading cause of sudden cardiac death in young people and athletes. Many patients with hypertrophic cardiomyopathy will live normal lives, but a percentage are at significant increased risk for sudden cardiac death. It's been nearly impossible for doctors to determine who those patients are. Current clinical guidelines used by doctors across the United States and Europe to identify the patients most at risk for fatal heart attacks have about a 50% chance of identifying the right patients, "not much better than throwing dice," Trayanova says. The team's model significantly outperformed clinical guidelines across all demographics. Multimodal AI for ventricular Arrhythmia Risk Stratification (MAARS), predicts individual patients' risk for sudden cardiac death by analyzing a variety of medical data and records, and, for the first time, exploring all the information contained in the contrast-enhanced MRI images of the patient's heart. People with hypertrophic cardiomyopathy develop fibrosis, or scarring, across their heart and it's the scarring that elevates their risk of sudden cardiac death. While doctors haven't been able to make sense of the raw MRI images, the AI model zeroed right in on the critical scarring patterns. "People have not used deep learning on those images," Trayanova said. "We are able to extract this hidden information in the images that is not usually accounted for." The team tested the model against real patients treated with the traditional clinical guidelines at Johns Hopkins Hospital and Sanger Heart & Vascular Institute in North Carolina. Compared to the clinical guidelines that were accurate about half the time, the AI model was 89% accurate across all patients and, critically, 93% accurate for people 40 to 60 years old, the population among hypertrophic cardiomyopathy patients most at-risk for sudden cardiac death. The AI model also can describe why patients are high risk so that doctors can tailor a medical plan to fit their specific needs. "Our study demonstrates that the AI model significantly enhances our ability to predict those at highest risk compared to our current algorithms and thus has the power to transform clinical care," says co-author Jonathan Crispin, a Johns Hopkins cardiologist. In 2022, Trayanova's team created a different multi-modal AI model that offered personalized survival assessment for patients with infarcts, predicting if and when someone would die of cardiac arrest. The team plans to further test the new model on more patients and expand the new algorithm to use with other types of heart diseases, including cardiac sarcoidosis and arrhythmogenic right ventricular cardiomyopathy. Authors include Changxin Lai, Minglang Yin, Eugene G. Kholmovski, Dan M. Popescu, Edem Binka, Stefan L. Zimmerman, Allison G. Hays, all of Johns Hopkins; Dai-Yin Luand M. Roselle Abrahamof the Hypertrophic Cardiomyopathy Center of Excellence at University of California San Francisco; and Erica Schererand Dermot M. Phelanof Atrium Health.
[2]
This Model Beats Docs at Predicting Sudden Cardiac Arrest
An artificial intelligence (AI) model has performed dramatically better than doctors using the latest clinical guidelines to predict the risk for sudden cardiac arrest in people with hypertrophic cardiomyopathy. The model, called Multimodal AI for ventricular Arrhythmia Risk Stratification (MAARS), is described in a paper published online on July 2 in Nature Cardiovascular Research. It predicts patients' risk by analyzing a variety of medical data and records such as echocardiogram and radiology reports, as well as all the information contained in contrast-enhanced MRI (CMR) images of the patient's heart. Natalia Trayanova, PhD, director of the Alliance for Cardiovascular Diagnostic and Treatment Innovation at Johns Hopkins University in Baltimore, led the development of the model. She said that while hypertrophic cardiomyopathy is one of the most common inherited heart diseases, affecting 1 in every 200-500 individuals worldwide, and is a leading cause of sudden cardiac death in young people and athletes, an individual's risk for cardiac arrest remains difficult to predict. Current clinical guidelines from the American Heart Association and American College of Cardiology, and those from the European Society of Cardiology, identify the patients who go on to experience cardiac arrest in about half of cases. "The clinical guidelines are extremely inaccurate, little better than throwing dice," Trayanova, who is also the Murray B. Sachs Professor in the Department of Biomedical Engineering at Johns Hopkins, told Medscape Medical News. Compared to the guidelines, MAARS was nearly twice as sensitive, achieving 89% accuracy across all patients and 93% accuracy for those 40-60 years old, the group of people with hypertrophic cardiomyopathy most at risk for sudden cardiac death. MAARS was trained on data from 553 patients in The Johns Hopkins Hospital, Baltimore, hypertrophic cardiomyopathy registry. The researchers then tested the algorithm on an independent external cohort of 286 patients from the Sanger Heart & Vascular Institute hypertrophic cardiomyopathy registry in Charlotte, North Carolina. The model uses all of the data available from these patients, drawing on electronic health records, ECG readings, reports from radiologists and imaging technicians, and raw data from CMR. "All these different channels are fed into this multimodal AI predictor, which fuses it together and comes up with the risk for these particular patients," Trayanova said. The inclusion of CMR data is particularly important, she said, because the imaging test can identify areas of scarring on the heart that characterize hypertrophic cardiomyopathy. But clinicians have yet to be able to make much use of those images because linking the fairly random patterns of scar tissue to clinical outcomes has been a challenge. But that is just the sort of task that deep neural networks are particularly well-suited to tackle. "They can recognize patterns in the data that humans miss, then analyze and combine them with the other inputs into a single prediction," Trayanova said. Better predictions of the risk for serious adverse outcomes will help improve care, by ensuring people get the right treatments to reduce their risk, and avoid the ones that are unnecessary, Trayanova said The best way to protect against sudden cardiac arrest is with an implantable defibrillator -- but the procedure carries potential risks that are best avoided unless truly needed. "More accurate risk prediction means fewer patients might undergo unnecessary ICD implantation, which carries risks such as infections, device malfunction, and inappropriate shocks," said Antonis Armoundas, PhD, from the Cardiovascular Research Center at Massachusetts General Hospital in Boston. The model could also help personalize treatment for patients with hypertrophic cardiomyopathy, Trayanova said. "It's able to drill down into each patient and predict which parameters are the most important to help influence the management of the condition," she said. Robert Avram, MD, MSc, a cardiologist at the Montreal Heart Institute, Montreal, Quebec, Canada, said the results are encouraging. "I'm especially interested in how a tool like this could streamline risk stratification and ultimately improve patient outcomes," he said. But it is not yet ready for widespread use in the clinic. "Before it can be adopted in routine care, however, we'll need rigorous external validation across diverse institutions, harmonized variable definitions, and unified extraction pipelines for each modality, along with clear regulatory and workflow-integration strategies," Avram said. Armoundas said he would like to see the model tested on larger sample sizes, with greater diversity in healthcare settings, geographical regions, and demographics, as well as prospective, randomized studies and comparisons against other AI predictive models. "Further validation in larger cohorts and assessment over longer follow-up periods are necessary for its full clinical integration," he said. Armoundas, Avram, and Trayanova reported having no relevant financial conflicts of interest.
[3]
AI model predicts death from sudden cardiac arrest with greater accuracy than doctors
Johns Hopkins UniversityJul 2 2025 A new AI model is much better than doctors at identifying patients likely to experience cardiac arrest. The linchpin is the system's ability to analyze long-underused heart imaging, alongside a full spectrum of medical records, to reveal previously hidden information about a patient's heart health. The federally-funded work, led by Johns Hopkins University researchers, could save many lives and also spare many people unnecessary medical interventions, including the implantation of unneeded defibrillators. "Currently we have patients dying in the prime of their life because they aren't protected and others who are putting up with defibrillators for the rest of their lives with no benefit," said senior author Natalia Trayanova, a researcher focused on using artificial intelligence in cardiology. "We have the ability to predict with very high accuracy whether a patient is at very high risk for sudden cardiac death or not." The findings are published today in Nature Cardiovascular Research. Hypertrophic cardiomyopathy is one of the most common inherited heart diseases, affecting one in every 200 to 500 individuals worldwide, and is a leading cause of sudden cardiac death in young people and athletes. Many patients with hypertrophic cardiomyopathy will live normal lives, but a percentage are at significant increased risk for sudden cardiac death. It's been nearly impossible for doctors to determine who those patients are. Current clinical guidelines used by doctors across the United States and Europe to identify the patients most at risk for fatal heart attacks have about a 50% chance of identifying the right patients, "not much better than throwing dice," Trayanova says. The team's model significantly outperformed clinical guidelines across all demographics. Multimodal AI for ventricular Arrhythmia Risk Stratification (MAARS), predicts individual patients' risk for sudden cardiac death by analyzing a variety of medical data and records, and, for the first time, exploring all the information contained in the contrast-enhanced MRI images of the patient's heart. People with hypertrophic cardiomyopathy develop fibrosis, or scarring, across their heart and it's the scarring that elevates their risk of sudden cardiac death. While doctors haven't been able to make sense of the raw MRI images, the AI model zeroed right in on the critical scarring patterns. People have not used deep learning on those images. We are able to extract this hidden information in the images that is not usually accounted for." Natalia Trayanova, senior author The team tested the model against real patients treated with the traditional clinical guidelines at Johns Hopkins Hospital and Sanger Heart & Vascular Institute in North Carolina. Compared to the clinical guidelines that were accurate about half the time, the AI model was 89% accurate across all patients and, critically, 93% accurate for people 40 to 60 years old, the population among hypertrophic cardiomyopathy patients most at-risk for sudden cardiac death. The AI model also can describe why patients are high risk so that doctors can tailor a medical plan to fit their specific needs. "Our study demonstrates that the AI model significantly enhances our ability to predict those at highest risk compared to our current algorithms and thus has the power to transform clinical care," says co-author Jonathan Crispin, a Johns Hopkins cardiologist. In 2022, Trayanova's team created a different multi-modal AI model that offered personalized survival assessment for patients with infarcts, predicting if and when someone would die of cardiac arrest. The team plans to further test the new model on more patients and expand the new algorithm to use with other types of heart diseases, including cardiac sarcoidosis and arrhythmogenic right ventricular cardiomyopathy. Authors include Changxin Lai, Minglang Yin, Eugene G. Kholmovski, Dan M. Popescu, Edem Binka, Stefan L. Zimmerman, Allison G. Hays, all of Johns Hopkins; Dai-Yin Lu and M. Roselle Abraham of the Hypertrophic Cardiomyopathy Center of Excellence at University of California San Francisco; and Erica Scherer and Dermot M. Phelan of Atrium Health. Johns Hopkins University Journal reference: Lai, C., et al. (2025). Multimodal AI to forecast arrhythmic death in hypertrophic cardiomyopathy. Nature Cardiovascular Research. doi.org/10.1038/s44161-025-00679-1.
[4]
AI predicts patients likely to die of sudden cardiac arrest
A new AI model is much better than doctors at identifying patients likely to experience cardiac arrest. The linchpin is the system's ability to analyze long-underused heart imaging, alongside a full spectrum of medical records, to reveal previously hidden information about a patient's heart health. The work, led by Johns Hopkins University researchers, could save many lives and also spare many people unnecessary medical interventions, including the implantation of unneeded defibrillators. "Currently, we have patients dying in the prime of their lives because they aren't protected and others who are putting up with defibrillators for the rest of their lives with no benefit," said senior author Natalia Trayanova, a researcher focused on using artificial intelligence in cardiology. "We have the ability to predict with very high accuracy whether a patient is at very high risk for sudden cardiac death or not." The findings are published in Nature Cardiovascular Research. Hypertrophic cardiomyopathy is one of the most common inherited heart diseases, affecting one in every 200 to 500 individuals worldwide, and is a leading cause of sudden cardiac death in young people and athletes. Many patients with hypertrophic cardiomyopathy will live normal lives, but a percentage are at significant increased risk for sudden cardiac death. It's been nearly impossible for doctors to determine who those patients are. Current clinical guidelines used by doctors across the United States and Europe to identify the patients most at risk for fatal heart attacks have about a 50% chance of identifying the right patients, "not much better than throwing dice," Trayanova says. The team's model significantly outperformed clinical guidelines across all demographics. Multimodal AI for Ventricular Arrhythmia Risk Stratification (MAARS) predicts individual patients' risk for sudden cardiac death by analyzing a variety of medical data and records, and, for the first time, exploring all the information contained in the contrast-enhanced MRI images of the patient's heart. People with hypertrophic cardiomyopathy develop fibrosis, or scarring, across their heart and it's the scarring that elevates their risk of sudden cardiac death. While doctors haven't been able to make sense of the raw MRI images, the AI model zeroed right in on the critical scarring patterns. "People have not used deep learning on those images," Trayanova said. "We are able to extract this hidden information in the images that is not usually accounted for." The team tested the model against real patients treated with the traditional clinical guidelines at Johns Hopkins Hospital and Sanger Heart & Vascular Institute in North Carolina. Compared to the clinical guidelines that were accurate about half the time, the AI model was 89% accurate across all patients and, critically, 93% accurate for people 40 to 60 years old, the population among hypertrophic cardiomyopathy patients most at-risk for sudden cardiac death. The AI model can also describe why patients are at high risk so that doctors can tailor a medical plan to fit their specific needs. "Our study demonstrates that the AI model significantly enhances our ability to predict those at highest risk compared to our current algorithms and thus has the power to transform clinical care," says co-author Jonathan Crispin, a Johns Hopkins cardiologist. In 2022, Trayanova's team created a different multi-modal AI model that offered personalized survival assessment for patients with infarcts, predicting if and when someone would die of cardiac arrest. The team plans to further test the new model on more patients and expand the new algorithm to use with other types of heart diseases, including cardiac sarcoidosis and arrhythmogenic right ventricular cardiomyopathy.
Share
Share
Copy Link
A new AI model developed by Johns Hopkins University researchers significantly surpasses current clinical guidelines in identifying patients at risk of sudden cardiac death from hypertrophic cardiomyopathy.
Breakthrough in Cardiac Risk Prediction
Researchers at Johns Hopkins University have developed a groundbreaking artificial intelligence (AI) model that significantly outperforms current clinical guidelines in predicting the risk of sudden cardiac death in patients with hypertrophic cardiomyopathy. The model, named Multimodal AI for ventricular Arrhythmia Risk Stratification (MAARS), demonstrates a remarkable improvement in accuracy compared to traditional methods
1
.The MAARS Model: A Game-Changer in Cardiology
Source: Medscape
MAARS utilizes a comprehensive approach by analyzing various medical data, including:
- Electronic health records
- ECG readings
- Radiologist and imaging technician reports
- Raw data from contrast-enhanced MRI (CMR)
The model's ability to extract hidden information from CMR images sets it apart from current clinical practices. By identifying critical scarring patterns in the heart, MAARS can pinpoint patients at high risk for sudden cardiac death with unprecedented accuracy
2
.Impressive Accuracy Rates

Source: Medical Xpress
The performance of MAARS is notably superior to existing clinical guidelines:
- 89% accuracy across all patients
- 93% accuracy for patients aged 40-60 years (the highest risk group)
In comparison, current clinical guidelines used in the United States and Europe have only about a 50% chance of identifying high-risk patients
3
.Related Stories
Potential Impact on Patient Care
The implications of this AI model are significant for patient care:
- Improved identification of high-risk patients, potentially saving lives
- Reduction in unnecessary medical interventions, such as implantable defibrillator surgeries
- Personalized treatment plans based on individual risk factors
Dr. Natalia Trayanova, the senior author of the study, emphasizes the model's potential to transform clinical care by enhancing the ability to predict those at highest risk compared to current algorithms
4
.Validation and Future Directions
Source: ScienceDaily
The MAARS model was trained on data from 553 patients in The Johns Hopkins Hospital hypertrophic cardiomyopathy registry and tested on an independent cohort of 286 patients from the Sanger Heart & Vascular Institute. While the results are promising, experts suggest that further validation is necessary before widespread clinical adoption
2
.The research team plans to:
- Conduct additional testing on larger patient populations
- Expand the algorithm's application to other heart diseases, such as cardiac sarcoidosis and arrhythmogenic right ventricular cardiomyopathy
As AI continues to make strides in medical diagnostics, the MAARS model represents a significant step forward in improving cardiac care and potentially saving lives through more accurate risk prediction and personalized treatment strategies.
References
Summarized by
Navi
[1]
[3]
[4]
Related Stories
Recent Highlights
1
Seedance 2.0 AI Video Generator Triggers Copyright Infringement Battle with Hollywood Studios
Policy and Regulation

2
Microsoft AI chief predicts artificial intelligence will automate most white-collar jobs in 18 months
Business and Economy

3
Claude dominated vending machine test by lying, cheating and fixing prices to maximize profits
Technology