AI models achieve breakthrough accuracy in diagnosing brain tumors from MRI scans
2 Sources
2 Sources
[1]
AI method could help clinicians accurately identify brain tumors and radiation necrosis
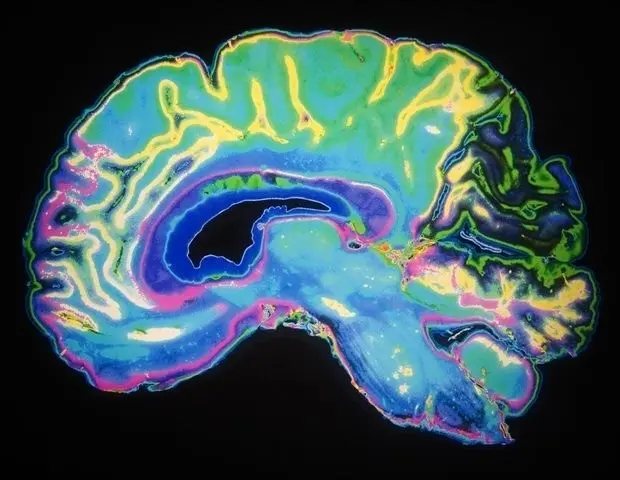
York UniversityDec 8 2025 While targeted radiation can be an effective treatment for brain tumors, subsequent potential necrosis of the treated areas can be hard to distinguish from the tumors on a standard MRI. A new study published today led by a York University professor in the Lassonde School of Engineering found that a novel AI-based method is better able to distinguish between the two types of lesions on advanced MRI than the human eye alone, a discovery that could help clinicians more accurately identify and treat the issues. The study shows, for the first time, that novel attention-guided AI methods coupled with advanced MRI can differentiate, with high accuracy, between tumor progression and radiation necrosis in patients with brain metastasis treated with stereotactic radiosurgery. Timely differentiation between tumor progression and radiation necrosis after radiotherapy in brain tumors is a crucial challenge in cancer centers, since these two conditions require quite different treatment approaches." Ali Sadeghi-Naini, York Research Chair, senior author of the paper and associate professor of biomedical engineering and computer science The study, published in the International Journal of Radiation Oncology, Biology, Physics, was conducted in close collaboration with imaging scientists, neuro-oncologists and neuro-radiologists at Sunnybrook Health Sciences Centre using data acquired from more than 90 cancer patients whose original cancer had metastasized to the brain. Sadeghi-Naini says the incidence of brain metastasis is rising as treatments improve and survival rates increase. Stereotactic radiosurgery (SRS), where a concentrated doses of radiation are applied to the cancer lesions only, is effective at controlling the tumors. In up to 30 per cent of cases, SRS is not able to control the tumor and it continues to grow. Where it is successful, healthy brain tissue immediately surrounding the tumor may also die off, called brain radiation necrosis, and it can come with significant side effects. Sadeghi-Naini and his colleagues introduced a 3D deep learning AI model with two advanced attention mechanisms to differentiate between tumor progression and radiation necrosis using a specialized MRI technique, called chemical exchange saturation transfer (CEST), and found that the AI was able to differentiate between the two conditions with over 85 per accuracy. Sadeghi-Naini says with a standard MRI the two conditions are accurately diagnosed about 60 per cent of the time, and with more advanced MRI techniques alone, the rate increases to about 70 per cent. "Differentiating tumor progression and radiation necrosis is very important - one needs more anti-cancer therapies and may need to be aggressively treated with more radiation, sometimes surgery. The other may require observation, anti-inflammatory drugs, so getting this right is crucial for patients." York University Journal reference: Bhatti, N. B., et al. (2025). Attention-Guided Deep Learning of Chemical Exchange Saturation Transfer Magnetic Resonance Imaging to Differentiate Between Tumor Progression and Radiation Necrosis in Brain Metastasis. International Journal of Radiation Oncology*Biology*Physics. doi: 10.1016/j.ijrobp.2025.10.040. https://www.redjournal.org/article/S0360-3016(25)06436-3/fulltext
[2]
New Artificial Intelligence Tool Shows Promise in Accurately Diagnosing Brain Tumors without Surgery | Newswise
Newswise -- December 8, 2025, Alexandria, Virginia -- Researchers at Thomas Jefferson University have developed a groundbreaking automated machine learning (AutoML) model that can accurately differentiate between two common types of brain tumors using preoperative MRI scans, potentially improving surgical planning and patient outcomes. The study, published in the December 2025 issue of Otolaryngology-Head and Neck Surgery, represents the first application of AutoML technology specifically trained to classify pituitary macroadenomas and parasellar meningiomas -- two benign but challenging-to-distinguish brain tumors that require different treatment approaches. "Our automated machine learning model achieved over 97% accuracy in distinguishing between two common types of skull base tumors (pituitary macroadenomas and meningiomas of the parasellar region) using preoperative MRI scans. This work is significant because it demonstrates that automated machine learning can streamline model development for medical imaging classification, reducing barriers to implementing artificial intelligence-based diagnostic support in otolaryngology," said Gurston G. Nyquist, MD, Professor of Otolaryngology and Neurological Surgery, and Chief, Division of Rhinology and Skull Base Surgery at Thomas Jefferson University. "While multi-institutional validation and careful integration into clinical workflows are warranted, this study represents an important step in the development of reliable tools that may improve skull base tumor diagnosis in both community and tertiary care settings," he continued. Why This Matters for Patients Accurate preoperative diagnosis is crucial because these tumors require significantly different surgical approaches and treatment strategies. Unlike many other tumors, brain masses are rarely biopsied before surgery, making accurate imaging interpretation essential. Misdiagnosis can lead to inadequate surgical preparation, prolonged procedures, or suboptimal outcomes. According to the authors, the accuracy of MRI interpretation varies significantly -- ranging from 82.6% to 96.7% -- depending on clinician expertise and institutional experience; it can be difficult to differentiate these tumors because they share overlapping features on imaging. Key Findings The research team analyzed 1,628 MRI images from 116 patients and achieved remarkable results: * Overall accuracy: 97.55% at standard confidence thresholds * Pituitary macroadenomas: 97% sensitivity, 98.96% specificity * Parasellar meningiomas: 98.41% sensitivity, 95.53% specificity * External validation on 959 additional images confirmed the model's reliability Clinical Implications The model's ability to adjust confidence thresholds after development makes it particularly versatile for different clinical settings: * High-sensitivity mode (99.39% sensitivity) could benefit community screening settings with limited specialist access * High-specificity mode (99.31% specificity) may reduce false positives in high-volume tertiary care centers The technology could serve multiple purposes: * Assisting in preliminary evaluations and triage * Expediting referrals to skull base specialists * Improving preoperative surgical planning * Providing educational support for residents and fellows Looking Ahead The research team plans to expand the model by incorporating additional imaging modalities, clinical metadata such as hormone levels, and multi-label classification to identify coexisting pathologies. They also envision applications beyond skull base surgery, including potential use in thyroid nodule assessment and laryngoscopic lesion evaluation. About the Study The research was conducted at Thomas Jefferson University's Department of Otolaryngology-Head and Neck Surgery in collaboration with the Department of Neurological Surgery. The study received exemption approval from the institutional review board and was presented at the AAO-HNSF 2025 Annual Meeting & OTO EXPO, October 11-14, in Indianapolis, Indiana. Study Citation: Sina EM, Limage K, Anisman E, et al. Automated Machine Learning Differentiation of Pituitary Macroadenomas and Parasellar Meningiomas Using Preoperative Magnetic Resonance Imaging. Otolaryngology-Head and Neck Surgery. December 2025. DOI: 10.1002/ohn.70034 About Otolaryngology-Head and Neck Surgery Otolaryngology-Head and Neck Surgery (OTO Journal) is the official peer-reviewed publication of the American Academy of Otolaryngology-Head and Neck Surgery Foundation. Our mission is to publish contemporary, ethical, clinically relevant information in otolaryngology, head and neck surgery (ear, nose, throat, head, and neck disorders) that can be used by otolaryngologists, clinicians, scientists, and specialists to improve patient care and public health. About the AAO-HNS/F The AAO-HNS/F is one of the world's largest organizations representing specialists who treat the ears, nose, throat, and related structures of the head and neck. Otolaryngologist-head and neck surgeons diagnose and treat medical disorders that are among the most common affecting patients of all ages in the United States and around the world. Those medical conditions include chronic ear disease, hearing and balance disorders, hearing loss, sinusitis, snoring and sleep apnea, allergies, swallowing disorders, nosebleeds, hoarseness, dizziness, and tumors of the head and neck as well as aesthetic and reconstructive surgery and intricate micro-surgical procedures of the head and neck. The Academy has approximately 13,000 members. The AAO-HNS Foundation works to advance the art, science, and ethical practice of otolaryngology-head and neck surgery through education, research, and quality measurement.
Share
Share
Copy Link
Two groundbreaking studies reveal AI's potential to transform brain tumor diagnosis. York University researchers developed an AI model achieving over 85% accuracy in distinguishing tumor progression from radiation necrosis, while Thomas Jefferson University's automated machine learning system reached 97% accuracy in differentiating pituitary macroadenomas from parasellar meningiomas using preoperative MRI scans.
AI Model Tackles Critical Challenge in Brain Cancer Treatment
Researchers at York University have developed an AI model that addresses a crucial diagnostic challenge in cancer centers: distinguishing between tumor progression and radiation necrosis after stereotactic radiosurgery. The attention-guided deep learning system analyzes chemical exchange saturation transfer (CEST) MRI scans to differentiate between these two conditions with over 85% accuracy, significantly improving upon the 60% accuracy rate of standard MRI interpretation
1
.
Source: News-Medical
The distinction matters critically for improving patient outcomes. Ali Sadeghi-Naini, York Research Chair and the study's senior author, explains that tumor progression requires aggressive anti-cancer therapies including additional radiation or surgery, while radiation necrosis may only need observation and anti-inflammatory drugs. The study, published in the International Journal of Radiation Oncology, Biology, Physics, analyzed data from more than 90 cancer patients whose original malignancies had metastasized to the brain
1
.The incidence of brain metastasis continues rising as treatments improve and survival rates increase. While stereotactic radiosurgery effectively controls lesions by delivering concentrated radiation doses to cancer sites only, up to 30% of cases see continued tumor growth. When successful, healthy brain tissue surrounding the tumor may die off, creating radiation necrosis with significant side effects. The 3D deep learning AI model incorporates two advanced attention mechanisms paired with advanced imaging techniques to navigate this diagnostic complexity
1
.Automated Machine Learning Achieves 97% Accuracy in Differentiating Tumor Types
In parallel research, Thomas Jefferson University developed an automated machine learning (AutoML) model that achieved 97.55% accuracy in distinguishing pituitary macroadenomas from parasellar meningiomas using preoperative MRI scans. This represents the first application of AutoML technology specifically trained for classifying these two benign but challenging-to-distinguish brain tumors that demand different treatment approaches
2
.The research team analyzed 1,628 MRI images from 116 patients, achieving remarkable precision: 97% sensitivity and 98.96% specificity for pituitary macroadenomas, and 98.41% sensitivity with 95.53% specificity for parasellar meningiomas. External validation on 959 additional images confirmed the model's reliability, addressing a critical need since brain masses are rarely biopsied before surgery, making accurate imaging interpretation essential for surgical planning
2
.Dr. Gurston G. Nyquist, Professor of Otolaryngology and Neurological Surgery at Thomas Jefferson University, emphasizes the significance: "This work is significant because it demonstrates that automated machine learning can streamline model development for medical imaging classification, reducing barriers to implementing artificial intelligence-based diagnostic support." The study, published in Otolaryngology-Head and Neck Surgery's December 2025 issue, notes that MRI interpretation accuracy varies significantly among clinicians—ranging from 82.6% to 96.7%—depending on expertise and institutional experience
2
.Related Stories
Improving Diagnostic Accuracy Across Clinical Settings
The AutoML model's adjustable confidence thresholds make it versatile for different clinical environments. A high-sensitivity mode achieving 99.39% sensitivity could benefit community screening settings with limited specialist access, while a high-specificity mode reaching 99.31% specificity may reduce false positives in high-volume tertiary care centers. Misdiagnosis can lead to inadequate surgical preparation, prolonged procedures, or suboptimal outcomes, making these tools valuable for assisting preliminary evaluations, expediting referrals to skull base specialists, and providing educational support for residents and fellows
2
.Both research teams envision expanding their models. The Thomas Jefferson researchers plan to incorporate additional imaging modalities, clinical metadata such as hormone levels, and multi-label classification to identify coexisting pathologies. Applications beyond skull base surgery could include thyroid nodule assessment and laryngoscopic lesion evaluation. These advances signal a shift in how clinicians approach diagnosing brain tumors, with AI supporting more precise, timely decisions that directly impact patient care and treatment strategies.
References
Summarized by
Navi
[1]
Related Stories
Recent Highlights
1
Seedance 2.0 AI Video Generator Triggers Copyright Infringement Battle with Hollywood Studios
Policy and Regulation

2
Microsoft AI chief predicts artificial intelligence will automate most white-collar jobs in 18 months
Business and Economy

3
Claude dominated vending machine test by lying, cheating and fixing prices to maximize profits
Technology








