AI Revolutionizes Heart Disease Detection: From ECGs to Hidden Conditions
6 Sources
6 Sources
[1]
AI Can Spot Lurking Heart Condition
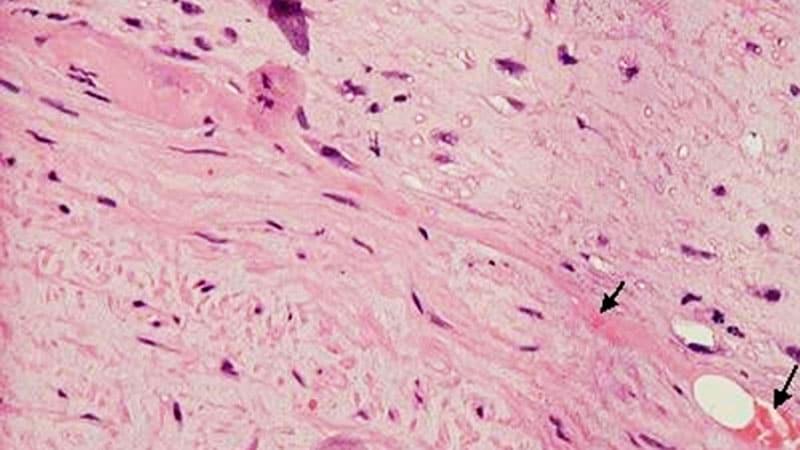
Artificial intelligence can detect cardiac amyloidosis from a short video of a heartbeat, according to new research in the European Heart Journal. Cardiac amyloidosis results when misshaped or misfolded proteins lodge throughout the heart, forcing it to work harder to pump blood. The condition can lead to thicker heart walls, is more common in older adults, and has features similar to those of hypertensive heart disease or aortic stenosis. Diagnosis is challenging, particularly in earlier disease stages, when thicker heart walls are not apparent on an echocardiogram. "If the patient has symptoms we can't explain and if the echo isn't quite normal, it would be reasonable to apply this AI model to see if they have amyloid," said Patricia Pellikka, MD, the Betty Knight Scripps Professor of Cardiovascular Disease Clinical Research at Mayo Clinic in Rochester, Minnesota, and a co-author of the new study. Those symptoms could be nonspecific, such as shortness of breath, fatigue, or swollen ankles, Pellikka said. Cardiac amyloidosis is definitively diagnosed with a biopsy or blood and urine analysis. Although rare, the number of cases appears to be rising. The prevalence rate rose from 8 to 17 per 100,000 person-years from 2000 to 2012, according to an analysis published in Circulation: Heart Failure. A 2025 analysis by researchers at Mayo Clinic found an overall prevalence of cardiac amyloidosis of 1.25% among more than 30,000 people who received an echocardiogram, with a greater incidence in people aged 80-89 years than among those aged 60-69. "Delays in diagnosis are very common with this disease," said Jeremy Slivnick, MD, a cardiologist at the University of Chicago who helped conduct the latest research. In many cases, a year or more will elapse between the first appearance of symptoms and a diagnosis of amyloidosis, at which point the disease is harder to control, he said. The new study validates previous research that led to the 2024 approval of the technology -- EchoGo Amyloidosis -- in the United States on a diverse population that spanned 18 global research sites. And the research shows that the AI model has broad applicability, Slivnick added. ""This is now an FDA-approved product," Slivnick said. "It's really critical that it works on everyone." Pellikka and her colleagues at Mayo previously worked with Ultromics, the Oxford, UK-based biotech firm that markets EchoGo Amyloidosis, to create an AI algorithm that distinguishes cardiac amyloidosis from other types of heart disease. They fed video clips of echocardiograms of people diagnosed with the disorder into the tool, as well as video clips of people with other heart conditions. These clips showed the heart's four chambers during heartbeats. The new retrospective study tested the AI tool at 18 global sites, with 597 echo videos of people with cardiac amyloidosis and 2122 videos of people with other heart conditions. The AI model effectively spotted all subtypes of amyloidosis in the dataset, with an area under the receiver-operating characteristic curve (AUROC) of 0.93, a sensitivity of 85% for identifying patients with the condition, and a specificity of 93% for finding those without the disorder. An apical four-chamber view of a patient with newly diagnosed hereditary ATTR amyloidosis. The patient had presented with heart failure with preserved ejection fraction. This videoclip was among those used to build the model. Video courtesy of Mayo Clinic/Ultromics Compared with other commonly used diagnostic tests for the condition, including concentrations of transthyretin (which can form amyloid deposits) and measurements of cardiac wall thickness, the AI model spotted more cases of concern. The AUROC for the AI model was 0,93, compared to an AUROC of 0.73 for transthyretin concentration and an AUROC of 0.80 for increased mediation. "Now we've got therapies for amyloid cardiomyopathy, but they work best if they're applied early in the natural history of the disease. We should be getting people on the treatment they need," Pellikka said. Several options exist. The FDA has approved three drugs for the treatment of cardiac amyloidosis, each of which can stop further production of amyloid deposits but do not reverse the damage already done. These drugs are tafamidis (Vyndamax), acoramidis (Attruby), and vutrisiran (Amvuttra). Amyloidosis "is a progressive disease. As of now we don't have anything to reverse the pathology, so the more protein that deposits in the heart, the worse these patients do," said David Snipelisky, MD, an advanced heart failure and transplant cardiologist at Cleveland Clinic in Weston, Florida. Heart transplants are sometimes an option, Snipelisky said, but in other cases only the medications meant to stop amyloid production are possible. Representatives of any echo lab can upload video clips of suspected cases of cardiac amyloidosis to a secure site maintained by the company, Pellikka said, and receive a result of whether amyloidosis is likely, unlikely, or indeterminate. Although the latest findings show the potential of the algorithm to diagnose cardiac amyloidosis from a single echo image, the next step would be test the tool in a prospective clinical trial, Snipelisky said. Snipelisky reported no relevant financial conflicts of interest. Slivnick reported relationships with GE Healthcare, Pfizer, and BridgeBio. Pellikka reported funding from the National Institutes of Health, Ultromics, and Edwards Lifesciences.
[2]
AI-powered ECG model outperforms doctors in detecting hidden heart disease
By Vijay Kumar MalesuReviewed by Susha Cheriyedath, M.Sc.Jul 21 2025 A breakthrough AI model can spot silent structural heart disease from a simple ECG, promising to catch dangerous conditions earlier, streamline patient care, and close the diagnostic gap missed by traditional screening. Study: Detecting structural heart disease from electrocardiograms using AI. Image Credit: DC Studio / Shutterstock In a recent study published in the journal Nature, a group of researchers investigated whether an artificial intelligence (AI) electrocardiogram (ECG) model can reliably detect diverse structural heart diseases (SHDs) across various hospitals and care settings, outperforming standard physician review. The model, called EchoNext, was developed as a multitask classifier to address collinearity among different SHD component labels. Background Every minute, another United States (US) patient enters the hospital with symptoms that may mask underlying SHD. Treating SHD already drains the nation of more than 100 billion dollars each year. Yet, an estimated 6.4% of older adults carry clinically significant valvular heart disease (VHD) that has never been diagnosed, in addition to 4.9% already diagnosed, making the total prevalence over 11%. Early echocardiography saves lives, but ultrasound labs, trained readers, and patient travel costs remain barriers, leaving busy clinicians guessing whom to scan. Large-scale digital ECG archives and modern AI offer a low-cost alternative: if one ten-second ECG could reliably uncover silent disease, scarce imaging resources could be directed to those who need them most. Further research is needed to determine whether algorithm-guided screening improves survival and equity. Additionally, the paper discusses potential deployment strategies for such models, including both "gatekeeper" and "safety net" applications, each with unique benefits and trade-offs for clinical practice. About the study Investigators assembled 1,245,273 paired ECG-echocardiogram records from 230,318 adults treated between 2008 and 2022 at eight NewYork-Presbyterian (NYP) hospitals, reserving patient-level splits for training, validation, and testing. SHD was labeled when any guideline defined abnormality was present with left ventricular ejection fraction (LVEF) ≤ 45%, left ventricular wall thickness ≥ 1.3 cm, moderate or worse right ventricular dysfunction, pulmonary artery systolic pressure (PASP) ≥ 45 mm Hg, or tricuspid regurgitation jet velocity ≥ 3.2 m/s as an alternative pulmonary hypertension definition, moderate or worse regurgitation/stenosis of any valve, or a moderate/large pericardial effusion. The authors note these thresholds are somewhat arbitrary, as different studies and guidelines may use varying cutoffs. A convolutional neural network named EchoNext ingested the raw 12-lead waveform, along with seven routine ECG parameters and age/sex data. Performance was first measured on a held-out NYP test set, and then on external cohorts from Cedars-Sinai, the Montreal Heart Institute, and the University of California, San Francisco. Generalization across age, sex, race, ethnicity, and clinical context was assessed. Silent "shadow" deployment ran EchoNext on 84,875 consecutive ECGs from patients without previous echocardiography, storing scores but not influencing care. Finally, a single-site pilot, Detecting Structural Heart Disease Using Deep Learning on an Electrocardiographic Waveform Array (DISCOVERY), prospectively invited adults with no recent imaging to undergo echocardiography stratified by a predecessor model's risk score; EchoNext was analyzed post hoc. Study results EchoNext, an AI-powered ECG model, excelled in retrospective analysis. Within the eight-hospital NYP test set, it detected composite SHD with an area under the receiver operating characteristic (AUROC) of 85.2% and an area under the precision-recall curve (AUPRC) of 78.5%. Accuracy remained consistent across academic and community campuses and did not falter when training and test sites were exchanged, demonstrating generalization. External validation at Cedars-Sinai Medical Center, the Montreal Heart Institute (MHI), and the University of California, San Francisco, yielded AUROC values of 78 to 80%, despite higher disease prevalence. Disease-specific performance: LVEF ≤ 45% achieved AUROC 90.4%, while PASP ≥ 45 millimeters of mercury reached 82.7%. The authors emphasize that AUPRC values for component diseases are highly dependent on the underlying disease prevalence and should not be directly compared across conditions or use cases. A 150-trace reader study compared EchoNext with thirteen cardiologists. Reviewing wide age, sex, waveform, and ECG intervals, physicians identified SHD correctly in 64% of cases. The AI alone achieved 77% accuracy, and when clinicians were shown the algorithmic risk score, their accuracy increased modestly to 69%, underscoring that the model captured prognostic patterns that were hidden from expert eyes. It is important to note that cardiologists in this assessment had access only to de-identified ECGs and routine parameters, without any clinical context, which is not typical of standard clinical care. To estimate clinical opportunity at scale, the team silently ran EchoNext on 124,027 ECGs recorded in 2023 from 84,875 adults who had never undergone echocardiography. The model flagged nine percent of traces as high risk. Usual care, nevertheless, left 45% of these individuals without follow-up imaging, suggesting that an estimated 1,998 cases of silent SHD might have been intercepted had the alert been live, based on modelled prevalence and sensitivity scenarios provided in the paper. Among the 15,094 patients who eventually received echocardiography, EchoNext preserved accuracy (AUROC 83%; AUPRC 81%) and delivered a positive predictive value of 74%, reinforcing its reliability in a contemporary workflow. The paper also provides modelled performance estimates at different prevalence scenarios and sensitivity thresholds, underscoring the practical implications for population-wide screening. Prospective evidence came from the DISCOVERY pilot, which recruited 100 imaging-naive adults. Post hoc EchoNext scoring revealed clear tiers, with previously unrecognized SHD present in 73% of high-risk participants, 28% of moderate-risk participants, and 6% of low-risk participants; moderate to severe left-sided VHD followed a similar gradient. These results illustrate the model's capacity to triage scarce echocardiography resources toward those most likely to benefit, while sparing low-risk individuals unnecessary testing. The original trial used a predecessor model (ValveNet) to stratify risk and recruit participants, and the EchoNext model was applied retrospectively to these participants for further analysis. Conclusions To summarize, EchoNext demonstrates that an AI-enhanced ECG can detect SHD associated with LVEF reduction, elevated PASP, and significant VHD, with AUROC and AUPRC metrics superior to those of cardiologists. By flagging high-risk patients for timely echocardiography, the algorithm promises to shrink diagnostic delay and the billion-dollar burden of SHD while maintaining equity across sites and demographics. However, the authors caution that AI-based screening may also carry potential risks, including patient anxiety from false positives or bias in clinical adoption, and highlight the need for further study of these aspects. The public release of code and data encourages independent validation; however, large pragmatic trials must verify that AI-guided ECG screening truly improves survival, quality of life, and healthcare value. Notably, the authors have released a large de-identified dataset and a benchmark AI model (the Columbia mini-model) to support further research and enable transparent comparison of future algorithms. Journal reference: Poterucha, T.J., Jing, L., Ricart, R.P., Adjei-Mosi, M., Finer, J., Hartzel, D., Kelsey, C., Long, A., Rocha, D., Ruhl, J.A. and vanMaanen, D. (2025). Detecting structural heart disease from electrocardiograms using AI. Nature. DOI: 10.1038/s41586-025-09227-0, https://www.nature.com/articles/s41586-025-09227-0
[3]
AI beats docs at identifying patients likely to die of cardiac arrest
A new AI model is much better than doctors at identifying patients likely to experience cardiac arrest. The linchpin is the system's ability to analyze long-underused heart imaging, alongside a full spectrum of medical records, to reveal previously hidden information about a patient's heart health. The research could save many lives and also spare many people unnecessary medical interventions, including the implantation of unneeded defibrillators. "Currently we have patients dying in the prime of their life because they aren't protected and others who are putting up with defibrillators for the rest of their lives with no benefit," says senior author Natalia Trayanova, a researcher focused on using artificial intelligence in cardiology. "We have the ability to predict with very high accuracy whether a patient is at very high risk for sudden cardiac death or not." Hypertrophic cardiomyopathy is one of the most common inherited heart diseases, affecting one in every 200 to 500 individuals worldwide, and is a leading cause of sudden cardiac death in young people and athletes. Many patients with hypertrophic cardiomyopathy will live normal lives, but a percentage are at significant increased risk for sudden cardiac death. It's been nearly impossible for doctors to determine who those patients are. Current clinical guidelines used by doctors across the United States and Europe to identify the patients most at risk for fatal heart attacks have about a 50% chance of identifying the right patients, "not much better than throwing dice," Trayanova says. The team's model significantly outperformed clinical guidelines across all demographics. Multimodal AI for ventricular Arrhythmia Risk Stratification (MAARS), predicts individual patients' risk for sudden cardiac death by analyzing a variety of medical data and records, and, for the first time, exploring all the information contained in the contrast-enhanced MRI images of the patient's heart. People with hypertrophic cardiomyopathy develop fibrosis, or scarring, across their heart and it's the scarring that elevates their risk of sudden cardiac death. While doctors haven't been able to make sense of the raw MRI images, the AI model zeroed right in on the critical scarring patterns. "People have not used deep learning on those images," Trayanova says. "We are able to extract this hidden information in the images that is not usually accounted for." The team tested the model against real patients treated with the traditional clinical guidelines at Johns Hopkins Hospital and Sanger Heart & Vascular Institute in North Carolina. Compared to the clinical guidelines that were accurate about half the time, the AI model was 89% accurate across all patients and, critically, 93% accurate for people 40 to 60 years old, the population among hypertrophic cardiomyopathy patients most at-risk for sudden cardiac death. The AI model also can describe why patients are high risk so that doctors can tailor a medical plan to fit their specific needs. "Our study demonstrates that the AI model significantly enhances our ability to predict those at highest risk compared to our current algorithms and thus has the power to transform clinical care," says co-author Jonathan Chrispin, a Johns Hopkins cardiologist. In 2022, Trayanova's team created a different multi-modal AI model that offered personalized survival assessment for patients with infarcts, predicting if and when someone would die of cardiac arrest. The team plans to further test the new model on more patients and expand the new algorithm to use with other types of heart diseases, including cardiac sarcoidosis and arrhythmogenic right ventricular cardiomyopathy. The findings appear in Nature Cardiovascular Research. Additional authors are from Johns Hopkins; the Hypertrophic Cardiomyopathy Center of Excellence at University of California, San Francisco; and Atrium Health. Support for the work came from the National Institutes of Health and a Leducq Foundation grant.
[4]
AI tool spots hidden heart disease using routine electrocardiogram data
With the help of artificial intelligence (AI), an inexpensive test found in many doctors' offices may soon be used to screen for hidden heart disease. Structural heart disease, including valve disease, congenital heart disease, and other issues that impair heart function, affects millions of people worldwide. Yet in the absence of a routine, affordable screening test, many structural heart problems go undetected until significant function has been lost. "We have colonoscopies, we have mammograms, but we have no equivalents for most forms of heart disease," says Pierre Elias, assistant professor of medicine and biomedical informatics at Columbia University Vagelos College of Physicians and Surgeons and medical director for artificial intelligence at NewYork-Presbyterian. Elias and researchers at Columbia University and NewYork-Presbyterian developed an AI-powered screening tool, EchoNext, that analyzes ordinary electrocardiogram (ECG) data to identify patients who should have an ultrasound (echocardiogram), a non-invasive test that is used to diagnose structural heart problems. In a study published in Nature, EchoNext accurately identified structural heart disease from ECG readings more often than cardiologists, including those who used AI to help interpret the data. "EchoNext basically uses the cheaper test to figure out who needs the more expensive ultrasound," says Elias, who led the study. "It detects diseases cardiologists can't from an ECG. We think that ECG plus AI has the potential to create an entirely new screening paradigm." The (echo)next step in cardiovascular screening The ECG is the most used cardiac test in health care. The test, which measures electrical activity in the heart, is typically used to detect abnormal heart rhythms, blocked coronary arteries, and prior heart attack. ECGs are inexpensive, non-invasive, and often administered to patients who are being treated for conditions unrelated to structural heart disease. While ECGs have their uses, they also have limitations. "We were all taught in medical school that you can't detect structural heart disease from an electrocardiogram," Elias says. Echocardiograms, which use ultrasound to obtain images of the heart, can be used to definitively diagnose valve disease, cardiomyopathy, pulmonary hypertension, and other structural heart problems that require medication or surgical treatment. EchoNext was designed to analyze ordinary ECG data to determine when follow-up with cardiac ultrasound is warranted. The deep learning model was trained on more than 1.2 million ECG-echocardiogram pairs from 230,000 patients. In a validation study across four hospital systems, including several NewYork-Presbyterian campuses, the screening tool demonstrated high accuracy in identifying structural heart problems, including heart failure due to cardiomyopathy, valve disease, pulmonary hypertension, and severe thickening of the heart. In a head-to-head comparison with 13 cardiologists on 3,200 ECGs, EchoNext accurately identified 77% of structural heart problems. In contrast, cardiologists making a diagnosis with the ECG data had an accuracy of 64%. Finding undiagnosed structural heart problems To see how well the tool worked in the real world, the research team ran EchoNext in nearly 85,000 patients undergoing ECG who had not previously had an echocardiogram. The AI tool identified more than 7,500 individuals -- 9% -- as at high-risk of having undiagnosed structural heart disease. The researchers then followed the patients over the course of a year to see how many were diagnosed with structural heart disease. (The patients' physicians were not aware of the EchoNext deployment so they were not influenced by its predictions). Among the individuals deemed high-risk by EchoNext, 55% went on to have their first echocardiogram. Of those, nearly three-quarters were diagnosed with structural heart disease -- twice the rate of positivity when compared to all people having their first echocardiogram without the benefit of AI. At the same positivity rate, if all the patients identified by EchoNext as high-risk had had an echocardiogram, about 2,000 additional patients may have been diagnosed with a potentially serious structural heart problem. "You can't treat the patient you don't know about," Elias says. "Using our technology, we may be able to turn the estimated 400 million ECGs that will be performed worldwide this year into 400 million chances to screen for structural heart disease and potentially deliver life-saving treatment at the most opportune time," Elias says. Elias and his team released a deidentified dataset to help other health systems improve screening for heart disease. The researchers have also launched a clinical trial to test EchoNext across eight emergency departments.
[5]
AI can identify hidden heart valve defects from a patient's EKG
An AI algorithm could help to predict which patients might develop significant heart problems years in advance, just based on EKG readings. In a study published in the European Heart Journal, researchers found that their AI could spot very early changes in the heart's structure from an EKG, a common test which shows the heart's electrical activity. The advanced algorithm could detect issues in the heart's valves -- which keep blood flowing in the correct direction through the heart's chambers -- even before the appearance of symptoms or physical changes that can be detected by ultrasound scans. The AI could accurately predict who would go on to develop significant leaks in the heart's mitral, tricuspid, or aortic valves -- conditions known as regurgitant valvular heart diseases. It was able to correctly identify the risk of a leaky heart valve in the years following the EKG (from high to low) in about 69%-79% of cases. People flagged as "high-risk" by the algorithm were up to 10 times more likely to develop these diseases than those classed as lower risk. According to the team from Imperial College London and Imperial College Healthcare NHS Trust, their AI-enhanced predictions could potentially transform doctors' approach to treating heart valve disease. It's estimated that 41 million people worldwide, including 1.5 million people in the U.K., live with these heart valve diseases, which can lead to heart failure, hospital admissions and death. Early diagnosis is key for successful treatment. But the symptoms, which can include shortness of breath, dizziness, feeling tired and having heart palpitations, can be easily confused with other causes, while some patients don't show any symptoms until the disease is advanced. Earlier detection Dr. Arunashis Sau, one of the study leads, Academic Clinical Lecturer at Imperial College London's National Heart and Lung Institute, and cardiology registrar at Imperial College Healthcare NHS Trust said, "Our hearts are incredibly complex and hard-working organs, but we rarely give them much consideration unless something goes wrong. By the time symptoms and structural changes appear in the heart, it may be too late to do much about it. "Our work is harnessing AI to detect subtle changes at the earliest stage from a simple and common test, and we think this could be really transformative for doctors and patients. Rather than waiting for symptoms, or relying only on expensive and time-consuming imaging tests, we could use AI-enhanced EKGs to spot those most at risk earlier than ever before. "This means that many more people could get the care they need before their hidden condition affects their quality of life or becomes life-threatening." The study was part of an international collaboration led by researchers Drs. Sau and Dr. Fu Siong Ng and involving researchers in China, based at Shanghai's Zhongshan Hospital. AI models were trained using nearly 1 million EKG and heart ultrasound (echocardiogram) records from more than 400,000 patients in China. The technology was then tested on a separate group of more than 34,000 patients in the United States, showing that it works well across ethnically diverse populations and health care systems. Issues with heart valves may first appear as very small changes to the heart's electrical activity which are not apparent to doctors. These electrical changes become larger but by this point, symptoms have often started to develop. The AI system can detect these subtle electrical patterns much earlier, hopefully before symptoms develop at all. Dr. Ng, the senior author, Reader in Cardiac Electrophysiology at the National Heart & Lung Institute at Imperial College London and a consultant cardiologist at Imperial College Healthcare NHS Trust and Chelsea and Westminster Hospital NHS Foundation Trust, said, "AI has enormous potential for improving health care around the world, but it requires huge amounts of data to train and test these algorithms. Our work is an example of the benefits of international collaboration in this fast-growing area. By training the model in an almost exclusively Chinese population and then testing in a U.S. cohort, we can show that our AI tool has the potential to be applied in various countries and settings around the world. This ultimately means it has the potential to help even more patients." Continued work The research follows on from the team's development of the related AI-EKG risk estimation model, known as AIRE, which can predict patients' risk of developing and worsening disease from an EKG. Other AI models from this project have been trained to analyze EKGs to predict problems such as female heart disease risk, health risks including early death, high blood pressure and type 2 diabetes.
[6]
Exclusive | New AI tool can detect 'hidden' heart disease 77% of the time,...
This new AI heart disease detector can't be beat. Structural heart disease (SHD) refers to defects in the heart's valves, wall or chambers that are present at birth or develop over time. These abnormalities can impair the heart's ability to pump blood effectively. SHD is sometimes described as "hidden" heart disease because it can progress without noticeable symptoms -- until there's a major event like a heart attack or stroke. Now, researchers at Columbia University and NewYork-Presbyterian have developed an AI- powered screening tool to identify who should undergo a key ultrasound used to diagnose structural heart problems. "There has been a growth in the number of AI models to detect, or opportunistically screen, disease," Dr. Pierre Elias, an assistant professor of medicine and biomedical informatics at Columbia's Vagelos College of Physicians and Surgeons, told The Post. "Some of the most exciting can look for coronary disease on CT scans or look at mammograms to help doctors find breast cancer more accurately," he added. "EchoNext is the first model to detect all forms of structural heart disease from ECGs." An electrocardiogram (ECG) is a quick, non-invasive procedure that measures the heart's electrical activity. It's one of the most frequently used cardiac tests, often ordered when patients experience symptoms such as shortness of breath, chest pain, palpitations or sudden loss of consciousness. While an ECG can detect some heart conditions, it's not reliable for catching SHD on its own. Enter EchoNext. The tool, fine-tuned over four years, analyzes ECG data to determine when follow-up with an echocardiogram is necessary. An echocardiogram is an ultrasound imaging test used to diagnose a range of heart conditions, including valve disorders and congenital heart defects. "EchoNext basically uses the cheaper test to figure out who needs the more expensive ultrasound," said Elias, study leader and medical director for artificial intelligence at NewYork-Presbyterian. "It detects diseases cardiologists can't from an ECG," he continued. "We think that ECG plus AI has the potential to create an entirely new screening paradigm." EchoNext was trained on over 1.2 million ECG-echocardiogram pairs from 230,000 patients. The tool accurately detected 77% of structural heart problems on 3,200 ECGs, outperforming 13 cardiologists who logged a 64% accuracy. EchoNext then identified over 7,500 people from a pool of nearly 85,000 study participants as high risk for undiagnosed SHD. The researchers followed the patients for a year without telling their physicians about the forewarning. Some 55% went on to have their first echocardiogram. Of those, almost three-quarters were diagnosed with SHD, a much higher positivity rate than usual. The findings were published Wednesday in the journal Nature. "The goal is to get the right patients to the right doctor and treatment sooner," Elias said. "The reality is many patients that need a cardiologist are often missed, and EchoNext helps facilitate getting these patients to the cardiologist who can then get the patient to the treatment they need." Looking ahead, Columbia has submitted a patent application on the EchoNext ECG algorithm. A clinical trial to test EchoNext in eight emergency departments is also underway.
Share
Share
Copy Link
Artificial intelligence models are transforming cardiac diagnostics, outperforming traditional methods in detecting various heart conditions from routine ECG data, promising earlier interventions and improved patient outcomes.
AI Surpasses Human Experts in Cardiac Diagnostics
Artificial intelligence (AI) is revolutionizing the field of cardiology, with new models demonstrating superior capabilities in detecting various heart conditions compared to traditional diagnostic methods. Recent studies have shown that AI-powered tools can identify hidden heart diseases from routine electrocardiograms (ECGs), outperforming human experts and potentially transforming patient care
1
2
3
.Detecting Cardiac Amyloidosis
Source: Medscape
Researchers have developed an AI model that can detect cardiac amyloidosis, a condition where misfolded proteins accumulate in the heart, from a short video of a heartbeat. The model, known as EchoGo Amyloidosis, achieved an impressive area under the receiver-operating characteristic curve (AUROC) of 0.93, with 85% sensitivity and 93% specificity
1
. This technology could significantly reduce diagnostic delays, which are common in amyloidosis cases and often lead to poorer outcomes.AI-Enhanced ECG Analysis for Structural Heart Disease

Source: Medical Xpress
A groundbreaking AI model called EchoNext has demonstrated the ability to detect structural heart diseases (SHDs) from standard ECG data. In a study involving over 1.2 million paired ECG-echocardiogram records, EchoNext achieved an AUROC of 85% for composite SHD detection
2
. The model outperformed cardiologists in a head-to-head comparison, correctly identifying 77% of structural heart problems compared to the doctors' 64% accuracy rate4
.Predicting Cardiac Arrest Risk
Another AI model has shown superior performance in identifying patients at risk of cardiac arrest. This system analyzes long-underused heart imaging alongside comprehensive medical records to reveal hidden information about a patient's heart health. The model achieved 89% accuracy across all patients and 93% accuracy for those aged 40 to 60, significantly outperforming current clinical guidelines
3
.Early Detection of Valve Defects

Source: Medical Xpress
Researchers have also developed an AI algorithm that can predict the development of significant heart valve problems years in advance, based solely on ECG readings. The model can accurately identify the risk of leaky heart valves in 69%-79% of cases, with high-risk individuals being up to 10 times more likely to develop these conditions
5
.Related Stories
Implications for Patient Care
These AI advancements have the potential to revolutionize cardiac care by enabling earlier interventions and more targeted treatments. For instance, the EchoNext model identified over 7,500 individuals at high risk of undiagnosed structural heart disease in a real-world deployment involving 85,000 patients
4
. This early detection could lead to timely interventions and improved patient outcomes.Challenges and Future Directions
While these AI models show great promise, their integration into clinical practice still faces challenges. Prospective clinical trials are needed to validate their effectiveness in real-world settings. Additionally, ensuring the generalizability of these models across diverse populations and healthcare systems remains a priority for researchers
2
5
.As AI continues to evolve, it holds the potential to create new screening paradigms for heart disease, potentially saving lives and reducing unnecessary medical interventions. The ongoing development and refinement of these technologies may soon lead to more widespread adoption in clinical settings, ushering in a new era of precision cardiology.
References
Summarized by
Navi
[1]
[4]
[5]
Related Stories
Recent Highlights
1
Seedance 2.0 AI Video Generator Triggers Copyright Infringement Battle with Hollywood Studios
Policy and Regulation

2
Microsoft AI chief predicts artificial intelligence will automate most white-collar jobs in 18 months
Business and Economy

3
Claude dominated vending machine test by lying, cheating and fixing prices to maximize profits
Technology