AI Tool for Skin Cancer Triage Receives Conditional NHS Approval
2 Sources
2 Sources
[1]
AI Tool for Skin Cancer Triage Gets Conditional NHS Approval
An artificial intelligence (AI) system for assessing suspicious skin lesions has been conditionally recommended by the National Institute for Health and Care Excellence (NICE) for NHS use in England. The tool, called Deep Ensemble for Recognition of Malignancy (DERM), can be used while further evidence is gathered. NICE said that the aim is to reduce delays for patients referred to the urgent suspected skin cancer pathway. Around one in three patients referred are not seen within the NHS 18-week target. DERM is designed to support teledermatology services following referral from primary care. Healthcare staff use a smartphone with a dermoscopic lens attachment to capture images of suspicious lesions. These are uploaded to DERM's secure online platform. The system uses a non-learning AI algorithm to analyse the images. It compares each image to a fixed database of known skin conditions, including: DERM provides a suspected diagnosis and triages the case. Patients with b enign lesions may be redirected to non-urgent pathways and receive written safety-netting advice. Suspicious lesions are reviewed virtually by a dermatologist. NICE said that comparative evidence suggests that DERM might be as accurate as face-to-face or teledermatology assessments, while easing pressure on dermatology services. Around 17,500 melanoma and 160,000 non-melanoma cancers are diagnosed each year in the UK. NHS dermatology services receive over one million referrals annually from primary care. Around 60% of these are urgent referrals for suspected skin cancer. However, only 6% of these are confirmed as cancer, with the remainder being either non-urgent or non-cancer cases. A shortage of consultant dermatologists has exacerbated delays. Some NHS trusts report having no dermatology consultants at all. As of July 2024, NHS England reported a referral-to-treatment backlog of 441,000 elective dermatology appointments. Only 63% met the 18-week treatment target. "DERM has shown promising results in its ability to accurately distinguish between cancerous and non-cancerous skin lesions," said Anastasia Chalkidou, director of NICE's Centre for Health Technology Evaluation. Evidence suggested that the system could halve the number of referrals to dermatologists within the urgent skin cancer pathway, while maintaining patient safety, she added. DERM will be used for the next 3 years while the NHS collects further evidence on its impact. NICE said it remains unclear whether the tool can also free up capacity for patients with non-cancer, non-urgent inflammatory skin conditions that still require face-to-face assessment. Also, current evidence is based largely on patients with white skin. Its performance in people with black or brown skin is less certain. To address this, patients from these groups will receive an additional review by a healthcare professional during the trial period. NICE will reconsider the evidence once the evaluation is complete and issue updated guidance.
[2]
Smartphones to detect skin cancer
Skin cancer checks will be carried out by AI using smartphones on the NHS. The National Institute for Health and Care Excellence (Nice) has backed the use of the technology to examine suspicious moles and lesions. The new artificial intelligence (AI) tool, Derm (deep ensemble for recognition of malignancy), can be used by healthcare workers using a smartphone with a high-quality magnifying lens attached. The images are then uploaded to an online platform, which uses AI to analyse the images. For patients whose moles or lesions are identified as potentially cancerous, a dermatologist will review the case. Nice said that early evidence suggested the tool, developed by Skin Analytics, could "approximately halve the number of referrals to dermatologists within the urgent skin cancer pathway". It had been "conditionally approved" for the next three years while further evidence was collected, Nice said. Dr Anastasia Chalkidou, healthtech programme director at Nice, said: "Derm has shown promising results in its ability to accurately distinguish between cancerous and non-cancerous skin lesions, with evidence suggesting it could halve the number of referrals to dermatologists within the urgent skin cancer pathway while maintaining patient safety," "Our evaluation shows this technology maintains diagnostic accuracy while reducing the burden on specialist dermatology services. By implementing this system within existing pathways, we can ensure patients get the right care more quickly." 'Slash waiting times' Ashley Dalton, minister for public health and prevention, said: "By embracing the power of AI, this exciting technology could help us slash waiting times, meaning that people with suspected skin cancer get the help they need, or peace of mind, faster." It comes as health experts issued a warning over sun cream ahead of the Bank Holiday weekend. Melanoma Focus said a large proportion of Britons are frequently letting themselves burn, putting themselves at a higher risk of skin cancer. Susanna Daniels, chief executive of Melanoma Focus, said: "It is essential that everyone understands the risks associated with sunburn and prioritises sun protection by using factor 30+ sunscreen, wearing a hat, seeking shade and covering up in the heat of the day." A poll by Melanoma Focus of 2,000 people aged 16 and over in the UK that almost half (49 per cent) said they are sunburnt at least once a year, with higher numbers reported in younger age groups. 'Concerning data' Ms Daniels said: "This data is extremely concerning as we know that more than five sunburns in your lifetime doubles your risk of melanoma, so burning every year has potentially long-term dangerous consequences. "Nearly nine in 10 melanomas are preventable, yet the UK has more deaths from melanoma per year than Australia." The poll also found that 19 per cent said they "rarely" wear sun cream in the UK between May and September, 8 per cent said they "never" use sun cream in the UK during this period. Almost one in 10 said they never wear sun cream at all. Reasons for avoiding sun cream in the UK included people not expecting to burn; forgetting to apply sun cream and eight per cent said sun cream is "too expensive".
Share
Share
Copy Link
The NHS in England has conditionally approved an AI system called DERM for assessing suspicious skin lesions, aiming to reduce delays in the urgent suspected skin cancer pathway.

AI-Powered Skin Cancer Triage Tool Gains Conditional NHS Approval
The National Institute for Health and Care Excellence (NICE) has conditionally recommended an artificial intelligence (AI) system called DERM (Deep Ensemble for Recognition of Malignancy) for use in the NHS in England. This innovative tool is designed to assess suspicious skin lesions and support teledermatology services, potentially revolutionizing skin cancer detection and triage
1
2
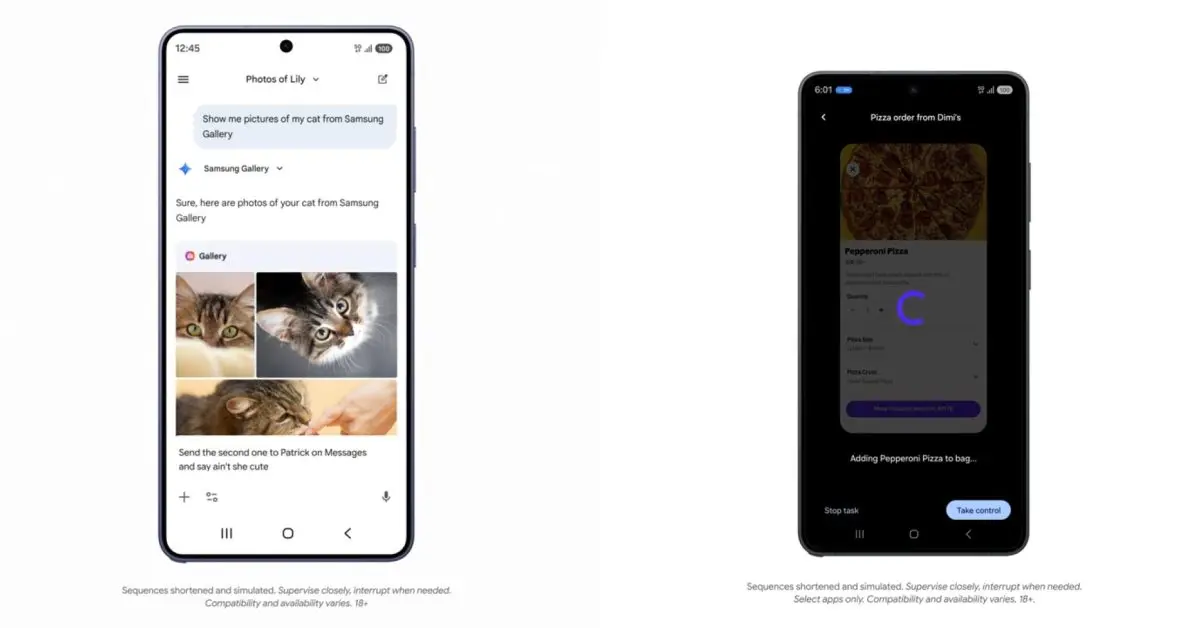
.How DERM Works
DERM utilizes a smartphone with a dermoscopic lens attachment to capture high-quality images of suspicious skin lesions. These images are then uploaded to a secure online platform where a non-learning AI algorithm analyzes them. The system compares each image to a fixed database of known skin conditions, providing a suspected diagnosis and triaging the case
1
.Potential Benefits and Impact
NICE suggests that DERM could significantly reduce delays for patients referred to the urgent suspected skin cancer pathway. Early evidence indicates that the tool might be as accurate as face-to-face or teledermatology assessments while easing pressure on dermatology services
1
.Dr. Anastasia Chalkidou, director of NICE's Centre for Health Technology Evaluation, stated, "DERM has shown promising results in its ability to accurately distinguish between cancerous and non-cancerous skin lesions, with evidence suggesting it could halve the number of referrals to dermatologists within the urgent skin cancer pathway while maintaining patient safety"
2
.Addressing NHS Challenges
The implementation of DERM comes at a crucial time for the NHS:
- High referral rates: NHS dermatology services receive over one million referrals annually from primary care, with about 60% being urgent referrals for suspected skin cancer
1
. - Low cancer confirmation rate: Only 6% of urgent referrals are confirmed as cancer
1
. - Consultant shortage: Some NHS trusts report having no dermatology consultants at all
1
. - Appointment backlog: As of July 2024, there was a backlog of 441,000 elective dermatology appointments, with only 63% meeting the 18-week treatment target
1
.
Trial Period and Further Evaluation
DERM will be used for the next three years while the NHS collects further evidence on its impact. NICE will reconsider the evidence once the evaluation is complete and issue updated guidance
1
2
.Related Stories
Limitations and Considerations
While promising, there are some limitations to consider:
- Performance on diverse skin tones: Current evidence is based largely on patients with white skin. Its performance in people with black or brown skin is less certain
1
. - Additional review: To address this limitation, patients from these groups will receive an additional review by a healthcare professional during the trial period
1
. - Impact on non-cancer cases: It remains unclear whether the tool can free up capacity for patients with non-cancer, non-urgent inflammatory skin conditions that still require face-to-face assessment
1
.
Conclusion
The conditional approval of DERM represents a significant step forward in leveraging AI technology to improve healthcare delivery and patient outcomes. As Ashley Dalton, minister for public health and prevention, noted, "By embracing the power of AI, this exciting technology could help us slash waiting times, meaning that people with suspected skin cancer get the help they need, or peace of mind, faster"
2
.References
Summarized by
Navi
[2]
Related Stories
Recent Highlights
1
Samsung unveils Galaxy S26 lineup with Privacy Display tech and expanded AI capabilities
Technology

2
Anthropic refuses Pentagon's ultimatum over AI use in mass surveillance and autonomous weapons
Policy and Regulation

3
AI models deploy nuclear weapons in 95% of war games, raising alarm over military use
Science and Research