AI Tool PhyloFrame Tackles Ancestral Bias in Genetic Research for Improved Precision Medicine
3 Sources
3 Sources
[1]
Computer engineers develop AI tool to account for ancestral diversity in genetic data
University of Florida researchers are addressing a critical gap in medical genetic research -- ensuring it better represents and benefits people of all backgrounds. Their work, led by Kiley Graim, Ph.D., an assistant professor in the Department of Computer & Information Science & Engineering, focuses on improving human health by addressing "ancestral bias" in genetic data, a problem that arises when most research is based on data from a single ancestral group. This bias limits advancements in precision medicine, Graim said, and leaves large portions of the global population underserved when it comes to disease treatment and prevention. To solve this, the team developed PhyloFrame, a machine-learning tool that uses artificial intelligence to account for ancestral diversity in genetic data. The goal is to improve how diseases are predicted, diagnosed, and treated for everyone, regardless of their ancestry. A paper describing the PhyloFrame method and how it showed marked improvements in precision medicine outcomes was published in Nature Communications. Graim's inspiration to focus on ancestral bias in genomic data evolved from a conversation with a doctor who was frustrated by a study's limited relevance to his diverse patient population. This encounter led her to explore how AI could help bridge the gap in genetic research. "I thought to myself, 'I can fix that problem,'" said Graim, whose research centers around machine learning and precision medicine and who is trained in population genomics. "If our training data doesn't match our real-world data, we have ways to deal with that using machine learning. They're not perfect, but they can do a lot to address the issue." By leveraging data from population genomics database gnomAD, PhyloFrame integrates massive databases of healthy human genomes with the smaller datasets specific to diseases used to train precision medicine models. The models it creates are better equipped to handle diverse genetic backgrounds. For example, it can predict the differences between subtypes of diseases like breast cancer and suggest the best treatment for each patient, regardless of patient ancestry. Processing such massive amounts of data is no small feat. The team uses UF's HiPerGator, one of the most powerful supercomputers in the country, to analyze genomic information from millions of people. For each person, that means processing 3 billion base pairs of DNA. "I didn't think it would work as well as it did," said Graim, noting that her doctoral student, Leslie Smith, contributed significantly to the study. "What started as a small project using a simple model to demonstrate the impact of incorporating population genomics data has evolved into securing funds to develop more sophisticated models and to refine how populations are defined." What sets PhyloFrame apart is its ability to ensure predictions remain accurate across populations by considering genetic differences linked to ancestry. This is crucial because most current models are built using data that does not fully represent the world's population. Much of the existing data comes from research hospitals and patients who trust the health care system. This means populations in small towns or those who distrust medical systems are often left out, making it harder to develop treatments that work well for everyone. She also estimated 97% of the sequenced samples are from people of European ancestry, due, largely, to national and state level funding and priorities, but also due to socioeconomic factors that snowball at different levels -- insurance impacts whether people get treated, for example, which impacts how likely they are to be sequenced. "Some other countries, notably China and Japan, have recently been trying to close this gap, and so there is more data from these countries than there had been previously, but still nothing like the European data," she said. "Poorer populations are generally excluded entirely." Thus, diversity in training data is essential, Graim said. "We want these models to work for any patient, not just the ones in our studies," she said. "Having diverse training data makes models better for Europeans, too. Having the population genomics data helps prevent models from overfitting, which means that they'll work better for everyone, including Europeans." Graim believes tools like PhyloFrame will eventually be used in the clinical setting, replacing traditional models to develop treatment plans tailored to individuals based on their genetic makeup. The team's next steps include refining PhyloFrame and expanding its applications to more diseases. "My dream is to help advance precision medicine through this kind of machine learning method, so people can get diagnosed early and are treated with what works specifically for them and with the fewest side effects," she said. "Getting the right treatment to the right person at the right time is what we're striving for."
[2]
UF researchers develop AI tool to tackle ancestral bias in precision medicine
University of FloridaMar 10 2025 University of Florida researchers are addressing a critical gap in medical genetic research - ensuring it better represents and benefits people of all backgrounds. Their work, led by Kiley Graim, Ph.D., an assistant professor in the Department of Computer & Information Science & Engineering, focuses on improving human health by addressing "ancestral bias" in genetic data, a problem that arises when most research is based on data from a single ancestral group. This bias limits advancements in precision medicine, Graim said, and leaves large portions of the global population underserved when it comes to disease treatment and prevention. To solve this, the team developed PhyloFrame, a machine-learning tool that uses artificial intelligence to account for ancestral diversity in genetic data. With funding support from the National Institutes of Health, the goal is to improve how diseases are predicted, diagnosed, and treated for everyone, regardless of their ancestry. A paper describing the PhyloFrame method and how it showed marked improvements in precision medicine outcomes was published Monday in Nature Communications. Graim's inspiration to focus on ancestral bias in genomic data evolved from a conversation with a doctor who was frustrated by a study's limited relevance to his diverse patient population. This encounter led her to explore how AI could help bridge the gap in genetic research. "I thought to myself, 'I can fix that problem,'" said Graim, whose research centers around machine learning and precision medicine and who is trained in population genomics. "If our training data doesn't match our real-world data, we have ways to deal with that using machine learning. They're not perfect, but they can do a lot to address the issue." By leveraging data from population genomics database gnomAD, PhyloFrame integrates massive databases of healthy human genomes with the smaller datasets specific to diseases used to train precision medicine models. The models it creates are better equipped to handle diverse genetic backgrounds. For example, it can predict the differences between subtypes of diseases like breast cancer and suggest the best treatment for each patient, regardless of patient ancestry. Processing such massive amounts of data is no small feat. The team uses UF's HiPerGator, one of the most powerful supercomputers in the country, to analyze genomic information from millions of people. For each person, that means processing 3 billion base pairs of DNA. "I didn't think it would work as well as it did," said Graim, noting that her doctoral student, Leslie Smith, contributed significantly to the study. "What started as a small project using a simple model to demonstrate the impact of incorporating population genomics data has evolved into securing funds to develop more sophisticated models and to refine how populations are defined." What sets PhyloFrame apart is its ability to ensure predictions remain accurate across populations by considering genetic differences linked to ancestry. This is crucial because most current models are built using data that does not fully represent the world's population. Much of the existing data comes from research hospitals and patients who trust the health care system. This means populations in small towns or those who distrust medical systems are often left out, making it harder to develop treatments that work well for everyone. She also estimated 97% of the sequenced samples are from people of European ancestry, due, largely, to national and state level funding and priorities, but also due to socioeconomic factors that snowball at different levels - insurance impacts whether people get treated, for example, which impacts how likely they are to be sequenced. Some other countries, notably China and Japan, have recently been trying to close this gap, and so there is more data from these countries than there had been previously but still nothing like the European data. Poorer populations are generally excluded entirely." Kiley Graim, Ph.D., Assistant Professor, Department of Computer & Information Science & Engineering, University of Florida Thus, diversity in training data is essential, Graim said. "We want these models to work for any patient, not just the ones in our studies," she said. "Having diverse training data makes models better for Europeans, too. Having the population genomics data helps prevent models from overfitting, which means that they'll work better for everyone, including Europeans." Graim believes tools like PhyloFrame will eventually be used in the clinical setting, replacing traditional models to develop treatment plans tailored to individuals based on their genetic makeup. The team's next steps include refining PhyloFrame and expanding its applications to more diseases. "My dream is to help advance precision medicine through this kind of machine learning method, so people can get diagnosed early and are treated with what works specifically for them and with the fewest side effects," she said. "Getting the right treatment to the right person at the right time is what we're striving for." Graim's project received funding from the UF College of Medicine Office of Research's AI2 Datathon grant award, which is designed to help researchers and clinicians harness AI tools to improve human health. University of Florida Journal reference: Smith, L. A., et al. (2025). Equitable machine learning counteracts ancestral bias in precision medicine. Nature Communications. doi.org/10.1038/s41467-025-57216-8.
[3]
AI tool to make genetic research more comprehensive
Their work, led by Kiley Graim, Ph.D., an assistant professor in the Department of Computer & Information Science & Engineering, focuses on improving human health by addressing "ancestral bias" in genetic data, a problem that arises when most research is based on data from a single ancestral group. This bias limits advancements in precision medicine, Graim said, and leaves large portions of the global population underserved when it comes to disease treatment and prevention. To solve this, the team developed PhyloFrame, a machine-learning tool that uses artificial intelligence to account for ancestral diversity in genetic data. With funding support from the National Institutes of Health, the goal is to improve how diseases are predicted, diagnosed, and treated for everyone, regardless of their ancestry. A paper describing the PhyloFrame method and how it showed marked improvements in precision medicine outcomes was published Monday in Nature Communications. Graim's inspiration to focus on ancestral bias in genomic data evolved from a conversation with a doctor who was frustrated by a study's limited relevance to his diverse patient population. This encounter led her to explore how AI could help bridge the gap in genetic research. "I thought to myself, 'I can fix that problem,'" said Graim, whose research centers around machine learning and precision medicine and who is trained in population genomics. "If our training data doesn't match our real-world data, we have ways to deal with that using machine learning. They're not perfect, but they can do a lot to address the issue." By leveraging data from population genomics database gnomAD, PhyloFrame integrates massive databases of healthy human genomes with the smaller datasets specific to diseases used to train precision medicine models. The models it creates are better equipped to handle diverse genetic backgrounds. For example, it can predict the differences between subtypes of diseases like breast cancer and suggest the best treatment for each patient, regardless of patient ancestry. Processing such massive amounts of data is no small feat. The team uses UF's HiPerGator, one of the most powerful supercomputers in the country, to analyze genomic information from millions of people. For each person, that means processing 3 billion base pairs of DNA. "I didn't think it would work as well as it did," said Graim, noting that her doctoral student, Leslie Smith, contributed significantly to the study. "What started as a small project using a simple model to demonstrate the impact of incorporating population genomics data has evolved into securing funds to develop more sophisticated models and to refine how populations are defined." What sets PhyloFrame apart is its ability to ensure predictions remain accurate across populations by considering genetic differences linked to ancestry. This is crucial because most current models are built using data that does not fully represent the world's population. Much of the existing data comes from research hospitals and patients who trust the health care system. This means populations in small towns or those who distrust medical systems are often left out, making it harder to develop treatments that work well for everyone. She also estimated 97% of the sequenced samples are from people of European ancestry, due, largely, to national and state level funding and priorities, but also due to socioeconomic factors that snowball at different levels -- insurance impacts whether people get treated, for example, which impacts how likely they are to be sequenced. "Some other countries, notably China and Japan, have recently been trying to close this gap, and so there is more data from these countries than there had been previously but still nothing like the European data," she said. "Poorer populations are generally excluded entirely." Thus, diversity in training data is essential, Graim said. "We want these models to work for any patient, not just the ones in our studies," she said. "Having diverse training data makes models better for Europeans, too. Having the population genomics data helps prevent models from overfitting, which means that they'll work better for everyone, including Europeans." Graim believes tools like PhyloFrame will eventually be used in the clinical setting, replacing traditional models to develop treatment plans tailored to individuals based on their genetic makeup. The team's next steps include refining PhyloFrame and expanding its applications to more diseases. "My dream is to help advance precision medicine through this kind of machine learning method, so people can get diagnosed early and are treated with what works specifically for them and with the fewest side effects," she said. "Getting the right treatment to the right person at the right time is what we're striving for." Graim's project received funding from the UF College of Medicine Office of Research's AI2 Datathon grant award, which is designed to help researchers and clinicians harness AI tools to improve human health.
Share
Share
Copy Link
University of Florida researchers develop an AI-powered tool called PhyloFrame to address ancestral bias in genetic data, aiming to improve precision medicine outcomes for diverse populations.

University of Florida Researchers Develop AI Tool to Address Ancestral Bias in Genetic Research
Researchers at the University of Florida have developed a groundbreaking AI tool called PhyloFrame to tackle a critical issue in medical genetic research: ancestral bias. Led by Dr. Kiley Graim, an assistant professor in the Department of Computer & Information Science & Engineering, the team aims to improve precision medicine outcomes for people of all backgrounds
1
.The Problem of Ancestral Bias
Ancestral bias in genetic data occurs when most research is based on data from a single ancestral group, typically of European descent. Dr. Graim estimates that 97% of sequenced samples come from people of European ancestry, due to funding priorities and socioeconomic factors
2
. This bias limits advancements in precision medicine and leaves large portions of the global population underserved in disease treatment and prevention.PhyloFrame: An AI Solution
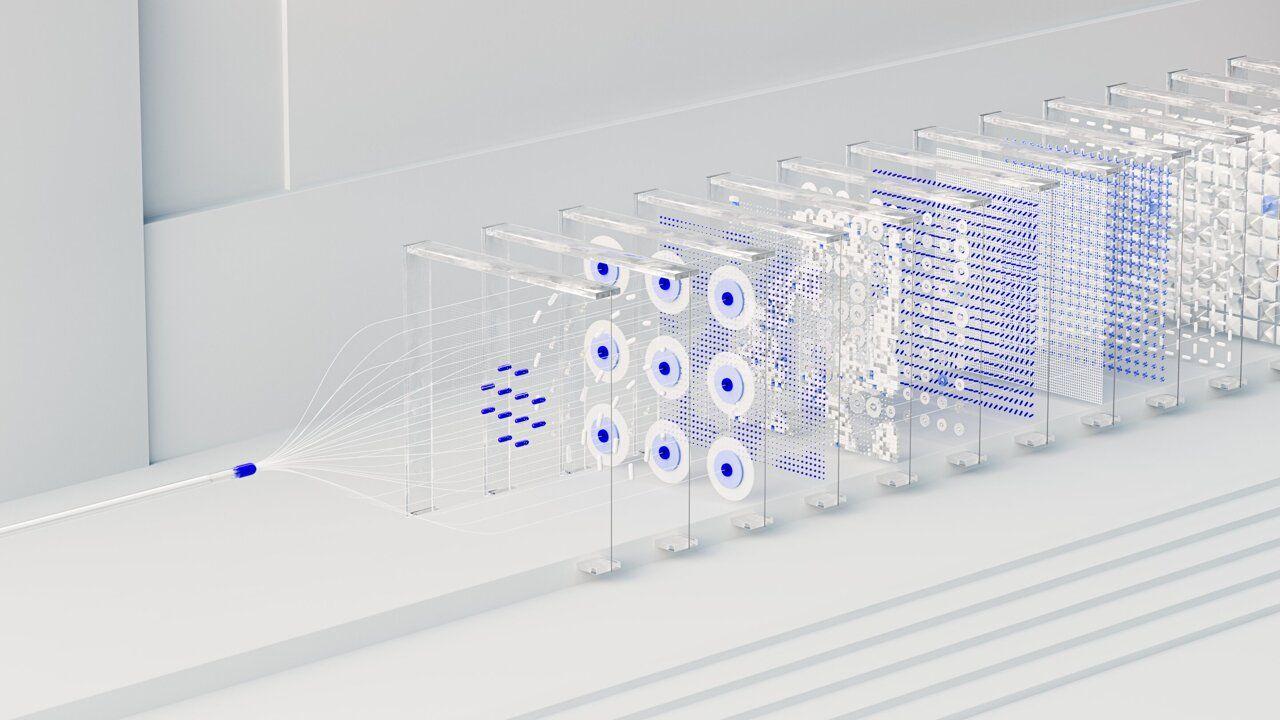
PhyloFrame is a machine-learning tool that uses artificial intelligence to account for ancestral diversity in genetic data. The tool integrates massive databases of healthy human genomes from the population genomics database gnomAD with smaller disease-specific datasets used to train precision medicine models
3
.Key features of PhyloFrame include:
- Ability to predict differences between disease subtypes
- Suggestion of best treatments for patients regardless of ancestry
- Improved accuracy across diverse populations
The Development Process
The development of PhyloFrame involved processing enormous amounts of genetic data. The team utilized UF's HiPerGator, one of the most powerful supercomputers in the country, to analyze genomic information from millions of people, processing 3 billion base pairs of DNA for each individual
1
.Related Stories
Implications for Precision Medicine
PhyloFrame's ability to consider genetic differences linked to ancestry sets it apart from current models. This is crucial because existing data often comes from research hospitals and patients who trust the healthcare system, leaving out populations in small towns or those who distrust medical systems
2
.Dr. Graim believes that tools like PhyloFrame will eventually be used in clinical settings, replacing traditional models to develop treatment plans tailored to individuals based on their genetic makeup
3
.Future Directions
The team's next steps include:
- Refining PhyloFrame
- Expanding its applications to more diseases
- Developing more sophisticated models
- Refining how populations are defined
The project received funding from the UF College of Medicine Office of Research's AI2 Datathon grant award, supporting the use of AI tools to improve human health
2
.As countries like China and Japan work to close the data gap, PhyloFrame represents a significant step towards more equitable and effective precision medicine, potentially revolutionizing how diseases are predicted, diagnosed, and treated for diverse populations worldwide.
References
Summarized by
Navi
[1]
[3]
Related Stories
AI Model Revolutionizes Genetic Disease Risk Prediction
29 Aug 2025•Science and Research

Researchers Caution Against Sole Reliance on AI in Healthcare, Advocate for Integrated Approach
17 Apr 2025•Health
AI-Assisted Genomic Studies Face Persistent Problems, Warn UW-Madison Researchers
05 Nov 2024•Science and Research

Recent Highlights
1
ByteDance's Seedance 2.0 AI video generator triggers copyright infringement battle with Hollywood
Policy and Regulation

2
Demis Hassabis predicts AGI in 5-8 years, sees new golden era transforming medicine and science
Technology

3
Nvidia and Meta forge massive chip deal as computing power demands reshape AI infrastructure
Technology





