Breakthrough in Alzheimer's Treatment: New Therapy Targets Tau Tangles
2 Sources
2 Sources
[1]
New therapy that targets and destroys tau tangles: A promising Alzheimer's disease treatment
Scientists have developed new potential therapies that selectively remove aggregated tau proteins, which are associated with Alzheimer's disease, and improve symptoms of neurodegeneration in mice. The team of scientists, from the Medical Research Council Laboratory of Molecular Biology (MRC LMB) in Cambridge, UK, and the UK Dementia Research Institute (UK DRI) at the University of Cambridge, say this promising approach could also be applied in future to other brain disorders driven by protein aggregation inside cells, such as motor neuron disease, Huntington's disease and Parkinson's disease. In two papers, published in Cell and Science, they demonstrate how utilizing the unique capabilities of a protein called TRIM21 gives the potential therapies two key advantages. Firstly, they only destroy the disease-linked tau aggregates, leaving healthy tau proteins intact. And secondly, the therapies remove already established tau aggregates in mice, not just preventing the formation of new aggregates. There are two main proteins that become misfolded and accumulate into aggregates in the brains of people affected by Alzheimer's disease: tau and amyloid. Amyloid aggregates form in the spaces between brain cells, where they are being targeted by new antibody therapies, such as lecanemab. In contrast, tau 'tangles' largely form inside nerve cells, although aggregates can spread from cell to cell, which is strongly associated with cognitive decline as the disease progresses. It is difficult for antibody therapies to access tau inside cells, therefore they do not remove existing tau aggregates inside cells -- at best they prevent aggregates from spreading. Other techniques for targeting tau inside cells, such as anti-sense oligonucleotides (ASOs), have been shown to reduce tau in promising early-stage clinical trials. However, they act on all tau in the brain and therefore also remove 'healthy' tau -- the long-term side-effects of this are not yet known. "Healthy" tau protein normally helps to provide structural support inside nerve cells in the brain -- acting as a type of scaffolding. This new technique for targeting tau tangles utilizes a 2010 discovery from Dr. Leo James' lab at the MRC Laboratory of Molecular Biology of the role of a unique protein called TRIM21, which is a key part of the immune response to viruses. Outside the cell, the body produces antibodies that bind to invading viruses. When the antibody-bound virus enters a cell, TRIM21 detects it and tags the virus as 'garbage,' handing it over to the cell's 'garbage chute,' the proteasome, for destruction. The same team, working across the UK DRI and MRC LMB, demonstrated in 2023 that TRIM21 could be re-purposed to destroy tau protein aggregates associated with Alzheimer's disease. By switching out antibodies that bind viruses for antibodies that bind to tau, TRIM21 was re-directed to send tau aggregates to be destroyed by the proteasome. TRIM21 is particularly suited to this because of a special feature -- a part of the protein called 'RING' that is activated only when two or more TRIM21 proteins cluster together. This means that it only activates and marks its target for destruction when TRIM21 proteins are bound to adjacent, aggregated tau proteins. In the new studies, scientists have used TRIM21 to create two new therapies to target tau aggregates. The first therapy, "RING-nanobody," combines a tau-binding nanobody -- a miniature version of an antibody -- with the TRIM21 RING. The second therapeutic, "RING-Bait," has the TRIM21 RING joined to a copy of the tau protein itself. The RING-linked tau protein acts as bait -- the aggregates incorporate it and TRIM21 RING gets incorporated as well. Once multiple RING-Baits are added to the aggregate, they become activated and cause the entire aggregate to be destroyed. The researchers delivered the DNA encoding the TRIM21 therapies into cells containing aggregated tau and found it cleared the tau tangles. As hoped, 'healthy' tau was left undamaged. Dr. Will McEwan, co-leader of the studies, from the UK Dementia Research Institute at the University of Cambridge said, "Tau aggregates are tucked away inside brain cells and very difficult to degrade. Critically, these new TRIM21-based therapies can be delivered directly inside cells, where the majority of tau aggregates reside. "We've found a way that not only degrades the tau aggregates, but leaves the healthy tau intact to do its job. The new strategy goes beyond what can be achieved with current ASO therapies that are being trialed, as it could avoid any potential long-term side-effects of eliminating normal tau." Since different neurodegenerative diseases can have different types of misfolded tau, they tested the therapies on cells containing aggregated tau proteins from brain tissue donated by people who had Alzheimer's disease or progressive supranuclear palsy, which have different misfolded tau structures. The RING-Bait therapy was able to prevent tau aggregation induced by proteins from both Alzheimer's and progressive supranuclear palsy patient brains. Dr. Leo James, co-leader of the studies, from the MRC Laboratory of Molecular Biology in Cambridge, said, "Neurodegenerative diseases can have tau proteins that misfold in many different ways, raising the possibility of needing a different treatment for every disease. A useful aspect of RING-Bait is because it is attached to a tau protein, it's a universal Trojan horse that should be incorporated into different types of tau aggregates exactly like the cell's own misfolding tau protein." For the treatment to work in an animal, it needs to not only get into the brain, but also get inside the cells within the brain. To do this, the researchers used a harmless virus that has previously been developed to deliver therapies like this, called an adeno-associated virus (AAV). It delivers DNA instructions to make the custom proteins inside brain cells. Elderly mice with tau protein aggregates were injected with a single dose of the gene therapy vector containing either the treatment, or a placebo. Within a few weeks, there was a significant reduction in the amount of aggregated tau in the brain cells of the treated animals. Importantly, in the mice given the RING-Bait treatment, the progression of their neurodegeneration symptoms slowed and they showed significantly better motor function, as assessed by an AI program that scored how well they ran. Dr. Lauren Miller, a study author, who worked across both the UK Dementia Research Institute and MRC Laboratory of Molecular Biology, said, "It was unknown whether specifically removing tau aggregates inside the cell would be enough to halt the progression of disease. "It is encouraging that a RING-Bait approach reduces disease severity in our model systems, as this suggests that the selective removal of tau aggregates is a valid therapeutic approach. Further work will be needed to demonstrate this beneficial effect is found across multiple models of human disease." Dr. Guido Papa, a study author, from MRC Laboratory of Molecular Biology, said, "The beauty of RING-Bait lies in its broad adaptability and the potential to tackle other conditions characterized by the accumulation of pathological protein clusters. "Other neurodegenerative diseases are caused by aggregates formed by other proteins, such as TDP43 in motor neuron disease and alpha-synuclein in Parkinson's disease. It is hoped that RING-Bait will allow the development of future therapies that directly target the aggregation process in these diseases." The scientists caution that these therapies still require a lot of development before they can be tested in humans, particularly developing an AAV vector that can safely and effectively deliver RING-nanobody or RING-bait therapies to cells throughout the human brain. Dr. Jonathan Benn, a study author, from the UK Dementia Research Institute at the University of Cambridge, said, "It's important to stress that although we have shown it works in a mouse model, this is a long way from a therapeutic that could be used in humans. It would need to be determined that it is safe to use TRIM21-based therapies in the human brain and that the treatments are effective in both removing aggregates and improving the course of disease. "Some AAV vectors are already approved for use in humans -- for instance in degenerative eye diseases and genetic diseases like spinal muscular atrophy. However, getting enough AAV into the adult brain remains a significant challenge -- the human brain is about 1,000 times bigger than a mouse brain. But this is a rapidly moving field and there are cutting edge gene delivery methods that we hope will allow our therapies to be delivered at scale in the future."
[2]
Scientists develop selective therapy for tau tangles
UK Research and InnovationSep 14 2024 Scientists have developed new potential therapies that selectively remove aggregated tau proteins, which are associated with Alzheimer's disease, and improve symptoms of neurodegeneration in mice. The team of scientists, from the Medical Research Council Laboratory of Molecular Biology (MRC LMB) in Cambridge, UK, and the UK Dementia Research Institute (UK DRI) at the University of Cambridge, say this promising approach could also be applied in future to other brain disorders driven by protein aggregation inside cells, such as motor neuron disease, Huntington's disease and Parkinson's disease. In two papers, published in Cell and Science, they demonstrated how utilising the unique capabilities of a protein called TRIM21 gives the potential therapies two key advantages. Firstly, they only destroyed the disease-linked tau aggregates, leaving healthy tau proteins intact. And secondly, the therapies removed already established tau aggregates in mice, not just preventing the formation of new aggregates. Tau tangles There are two main proteins that become misfolded and accumulate into aggregates in the brains of people affected by Alzheimer's disease: tau and amyloid. Amyloid aggregates form in the spaces between brain cells, where they are being targeted by new antibody therapies, such as lecanemab. In contrast, tau 'tangles' largely form inside nerve cells, although aggregates can spread from cell to cell, which is strongly associated with cognitive decline as the disease progresses. It is difficult for antibody therapies to access tau inside cells, therefore they do not remove existing tau aggregates inside cells - at best they prevent aggregates from spreading. Other techniques for targeting tau inside cells, such as anti-sense oligonucleotides (ASOs), have been shown to reduce tau in promising early-stage clinical trials. However, they act on all tau in the brain and therefore also remove 'healthy' tau - the long-term side-effects of this are not yet known. 'Healthy' tau protein normally helps to provide structural support inside nerve cells in the brain - acting as a type of scaffolding. Trimming Alzheimer's-linked proteins This new technique for targeting tau tangles utilises a 2010 discovery from Dr Leo James' lab at the MRC Laboratory of Molecular Biology of the role of a unique protein called TRIM21, which is a key part of the immune response to viruses. Outside the cell, the body produces antibodies that bind to invading viruses. When the antibody-bound virus enters a cell, TRIM21 detects it and tags the virus as 'garbage', handing it over to the cell's 'garbage chute', the proteasome, for destruction. The same team, working across the UK DRI and MRC LMB, demonstrated in 2023 that TRIM21 could be re-purposed to destroy tau protein aggregates associated with Alzheimer's disease. By switching out antibodies that bind viruses for antibodies that bind to tau, TRIM21 was re-directed to send tau aggregates to be destroyed by the proteasome. TRIM21 is particularly suited to this because of a special feature - a part of the protein called 'RING' that is activated only when two or more TRIM21 proteins cluster together. This means that it only activates and marks its target for destruction when TRIM21 proteins are bound to adjacent, aggregated tau proteins. New Trojan horse therapy for tau aggregates In the new studies, scientists have used TRIM21 to create two new therapies to target tau aggregates. The first therapy, 'RING-nanobody', combines a tau-binding nanobody - a miniature version of an antibody - with the TRIM21 RING. The second therapeutic, 'RING-Bait', has the TRIM21 RING joined to a copy of the tau protein itself. The RING-linked tau protein acts as bait - the aggregates incorporate it and TRIM21 RING gets incorporated as well. Once multiple RING-Baits are added to the aggregate, they become activated and causes the entire aggregate to be destroyed. The researchers delivered the DNA encoding the TRIM21 therapies into cells containing aggregated tau and found it cleared the tau tangles. As hoped, 'healthy' tau was left undamaged. Dr Will McEwan, co-leader of the studies, from the UK Dementia Research Institute at the University of Cambridge said: "Tau aggregates are tucked away inside brain cells and very difficult to degrade. Critically, these new TRIM21-based therapies can be delivered directly inside cells, where the majority of tau aggregates reside. We've found a way that not only degrades the tau aggregates, but leaves the healthy tau intact to do its job. The new strategy goes beyond what can be achieved with current ASO therapies that are being trialled, as it could avoid any potential long-term side-effects of eliminating normal tau." Dr. Will McEwan, UK Dementia Research Institute, University of Cambridge Since different neurodegenerative diseases can have different types of misfolded tau, they tested the therapies on cells containing aggregated tau proteins from brain tissue donated by people who had Alzheimer's disease or progressive supranuclear palsy, which have different misfolded tau structures. The RING-Bait therapy was able to prevent tau aggregation induced by proteins from both Alzheimer's and progressive supranuclear palsy patient brains. Dr Leo James, co-leader of the studies, from the MRC Laboratory of Molecular Biology in Cambridge, said: "Neurodegenerative diseases can have tau proteins that misfold in many different ways, raising the possibility of needing a different treatment for every disease. A useful aspect of RING-Bait is because it is attached to a tau protein, it's a universal Trojan horse that should be incorporated into different types of tau aggregates exactly like the cell's own misfolding tau protein." Mice walk better after therapy For the treatment to work in an animal, it needs to not only get into the brain, but also get inside the cells within the brain. To do this, the researchers used a harmless virus that has previously been developed to deliver therapies like this, called an adeno-associated virus (AAV). It delivers DNA instructions to make the custom proteins inside brain cells. Elderly mice with tau protein aggregates were injected with a single dose of the gene therapy vector containing either the treatment, or a placebo. Within a few weeks, there was a significant reduction in the amount of aggregated tau in the brain cells of the treated animals. Importantly, in the mice given the RING-Bait treatment, the progression of their neurodegeneration symptoms slowed and they showed significantly better motor function, as assessed by an AI programme that scored how well they ran. Dr Lauren Miller, a study author, who worked across both the UK Dementia Research Institute and MRC Laboratory of Molecular Biology, said: "It was unknown whether specifically removing tau aggregates inside the cell would be enough to halt the progression of disease. It is encouraging that a RING-Bait approach reduces disease severity in our model systems, as this suggests that the selective removal of tau aggregates is a valid therapeutic approach. Further work will be needed to demonstrate this beneficial effect is found across multiple models of human disease." Dr Guido Papa, a study author, from MRC Laboratory of Molecular Biology, said: "The beauty of RING-Bait lies in its broad adaptability and the potential to tackle other conditions characterised by the accumulation of pathological protein clusters. Other neurodegenerative diseases are caused by aggregates formed by other proteins, such as TDP43 in motor neuron disease and alpha-synuclein in Parkinson's disease. It is hoped that RING-Bait will allow the development of future therapies that directly target the aggregation process in these diseases." The scientists caution that these therapies still require a lot of development before they can be tested in humans, particularly developing an AAV vector that can safely and effectively deliver RING-nanobody or RING-bait therapies to cells throughout the human brain. Dr Jonathan Benn, a study author, from the UK Dementia Research Institute at the University of Cambridge, said: "It's important to stress that although we have shown it works in a mouse model, this is a long way from a therapeutic that could be used in humans. It would need to be determined that it is safe to use TRIM21-based therapies in the human brain and that the treatments are effective in both removing aggregates and improving the course of disease. "Some AAV vectors are already approved for use in humans - for instance in degenerative eye diseases and genetic diseases like spinal muscular atrophy. However, getting enough AAV into the adult brain remains a significant challenge - the human brain is about 1,000 times bigger than a mouse brain. But this is a rapidly moving field and there are cutting edge gene delivery methods that we hope will allow our therapies to be delivered at scale in the future." These studies were primarily funded by Wellcome, MRC, UK DRI, and The Lister Institute of Preventative Medicine. UK Research and Innovation Journal reference: Miller, L. V. C., et al. (2024) Co-opting templated aggregation to degrade pathogenic tau assemblies and improve motor function. Cell. doi.org/10.1016/j.cell.2024.08.024.
Share
Share
Copy Link
Scientists have developed a novel therapy that selectively destroys tau tangles in Alzheimer's disease. This groundbreaking approach shows promise in treating the neurodegenerative disorder without harming healthy brain cells.

A New Hope for Alzheimer's Patients
Researchers have made a significant breakthrough in the fight against Alzheimer's disease, developing a innovative therapy that specifically targets and destroys tau tangles, a hallmark of the neurodegenerative disorder. This groundbreaking approach, detailed in a recent study, offers new hope for millions of people affected by Alzheimer's worldwide
1
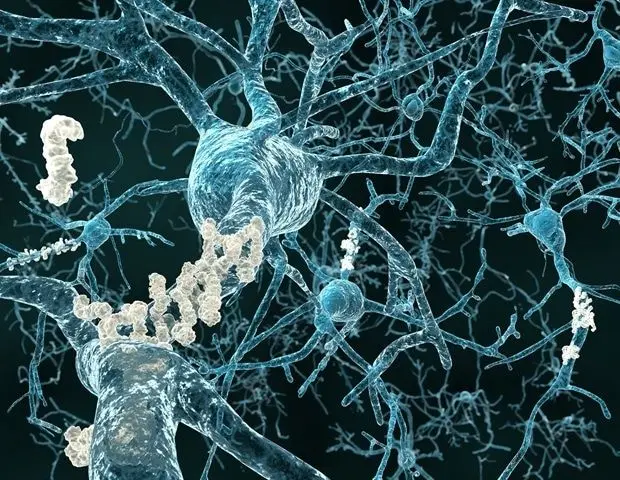
.Understanding Tau Tangles and Their Role in Alzheimer's
Tau tangles, along with amyloid plaques, are considered primary culprits in the progression of Alzheimer's disease. These abnormal accumulations of tau protein in the brain interfere with normal neuronal function, leading to cognitive decline and memory loss. Until now, effectively targeting these tangles without damaging healthy brain cells has been a significant challenge in Alzheimer's research
2
.The Breakthrough: Selective Tau Tangle Destruction
The newly developed therapy employs a novel approach that selectively identifies and eliminates tau tangles while leaving healthy neurons unharmed. This precision is crucial, as previous attempts to target tau proteins often resulted in unintended damage to normal brain cells, limiting their therapeutic potential
1
.Mechanism of Action
The therapy works by utilizing a specially designed antibody that recognizes and binds to the pathological form of tau protein found in tangles. Once bound, the antibody triggers a cellular response that leads to the destruction of the tau tangles. This process, known as antibody-dependent cellular phagocytosis, effectively clears the harmful protein aggregates from the brain
2
.Promising Results in Preclinical Studies
Initial studies conducted on animal models have shown remarkable results. Researchers observed a significant reduction in tau tangles and improvements in cognitive function in treated subjects. These findings suggest that the therapy could potentially slow or even halt the progression of Alzheimer's disease
1
.Related Stories
Implications for Future Alzheimer's Treatment
The development of this selective therapy represents a major step forward in Alzheimer's research. By specifically targeting tau tangles without affecting healthy brain tissue, this approach addresses one of the key challenges in treating the disease. If successful in human trials, it could lead to more effective treatments with fewer side effects than current options
2
.Next Steps: Human Clinical Trials
With the promising results from preclinical studies, researchers are now preparing for human clinical trials. These trials will be crucial in determining the safety and efficacy of the therapy in humans. Scientists are optimistic about the potential of this new approach to revolutionize Alzheimer's treatment and improve the lives of millions of patients and their families
1
.References
Summarized by
Navi
[1]
[2]
Related Stories
Recent Highlights
1
OpenAI Releases GPT-5.4, New AI Model Built for Agents and Professional Work
Technology

2
Anthropic takes Pentagon to court over unprecedented supply chain risk designation
Policy and Regulation

3
Meta smart glasses face lawsuit and UK probe after workers watched intimate user footage
Policy and Regulation