AI-Designed Proteins Revolutionize Cancer Immunotherapy: A Breakthrough in Precision Treatment
5 Sources
5 Sources
[1]
AI is designing proteins that could help treat cancer
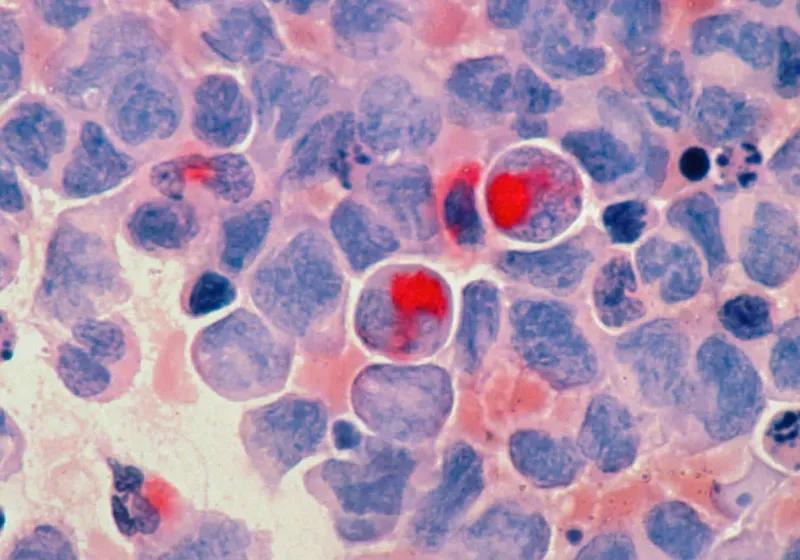
The proteins supercharge T cells' ability to target and destroy melanoma cells Using AI, scientists have built a "GPS" for cancer-fighting immune cells. It's a molecular navigation system that helped the cells lock onto cancer, kind of like Google Maps guiding travelers to a new address, researchers report July 24 in Science. At its core, the system relies on tiny proteins custom-designed by artificial intelligence. The approach, a form of immunotherapy, is "very much a proof-of-concept," says Timothy Jenkins, a medical biotechnologist at the Technical University of Denmark in Lyngby. But his team's end goal is to develop new therapies doctors can use to treat cancer -- perhaps even personalized for individual patients. "It's an exciting advance," says Stanley Riddell, an immunotherapy researcher at Fred Hutch Cancer Center in Seattle. Though the work is still in the early stages, it showcases the power of AI models for synthetic protein design, he says. Such models are "likely to generate a whole new class of therapeutics for a variety of diseases that will go beyond cancer." Earlier this year, in fact, Jenkins and his colleagues reported a similar AI advance in a different field of medicine: AI-designed proteins that could lead to improved antivenoms for snakebites. Now, the researchers have directed their AI systems toward a new destination: cancer. The team was looking for ways to rev up the cancer-seeking potential of immune cells called T cells. T cells can fight cancer on their own but sometimes have trouble recognizing the enemy. Jenkins' team genetically engineered T cells to carry tiny custom proteins on their surface. Those proteins act as the GPS, guiding T cells to their cancer target. The work riffs off other immunotherapy techniques, like CAR T-cell therapy and TCR therapy, which also try to boost immune cells' anti-cancer prowess. To design the custom proteins, the researchers relied on a trio of AI tools. First, the team inputted the structure of the cancer target into a generative AI model called RFdiffusion. That model had been trained on known protein structures and their amino acid sequences, the strings of building blocks that fold up into individual proteins. RFdiffusion proposed protein shapes that fit the target like a key fits a lock. A second AI model suggested strings of amino acids that, when folded into 3-D structures, would likely form the proposed shapes. Jenkins and his colleagues then blasted through tens of thousands of protein designs and, with the help of a third AI model that checked all that work, narrowed the designs down to 44 options that they tested in the lab. One appeared to be a winner. In lab experiments, human T cells engineered to have the AI-designed protein on their surface could rapidly kill melanoma cells and prevent the cancer from growing. The team's work is based on the computational protein design and structure prediction technologies that led to the 2024 Nobel Prize in chemistry. It takes as little as a day or two to come up with promising designs, Jenkins says, and just a few weeks to test them in the lab. That's faster than current methods, which can involve hunting through people's cells to pick out proteins, known as T cell receptors, naturally able to lock on to specific cancer targets. "It's extremely laborious," says Christopher Klebanoff, a medical oncologist and researcher at Memorial Sloan Kettering Cancer Center in New York City. The process can take months and even then "you can end up with nothing or a very, very small number of therapeutic candidates." Klebanoff thinks the new work is an important step, but he's curious how the AI-designed proteins will work inside the body. Before the researchers take their approach to clinical trials in humans, they'll need to do many more tests in the lab and in animals, which could take years, says Kristoffer Haurum Johansen, a synthetic immunologist also at the Technical University of Denmark. But for now, he says, his team's work "means that there's a potential new tool in the toolbox that we can use to design and develop new therapies."
[2]
AI turns immune cells into precision cancer killers -- in just weeks
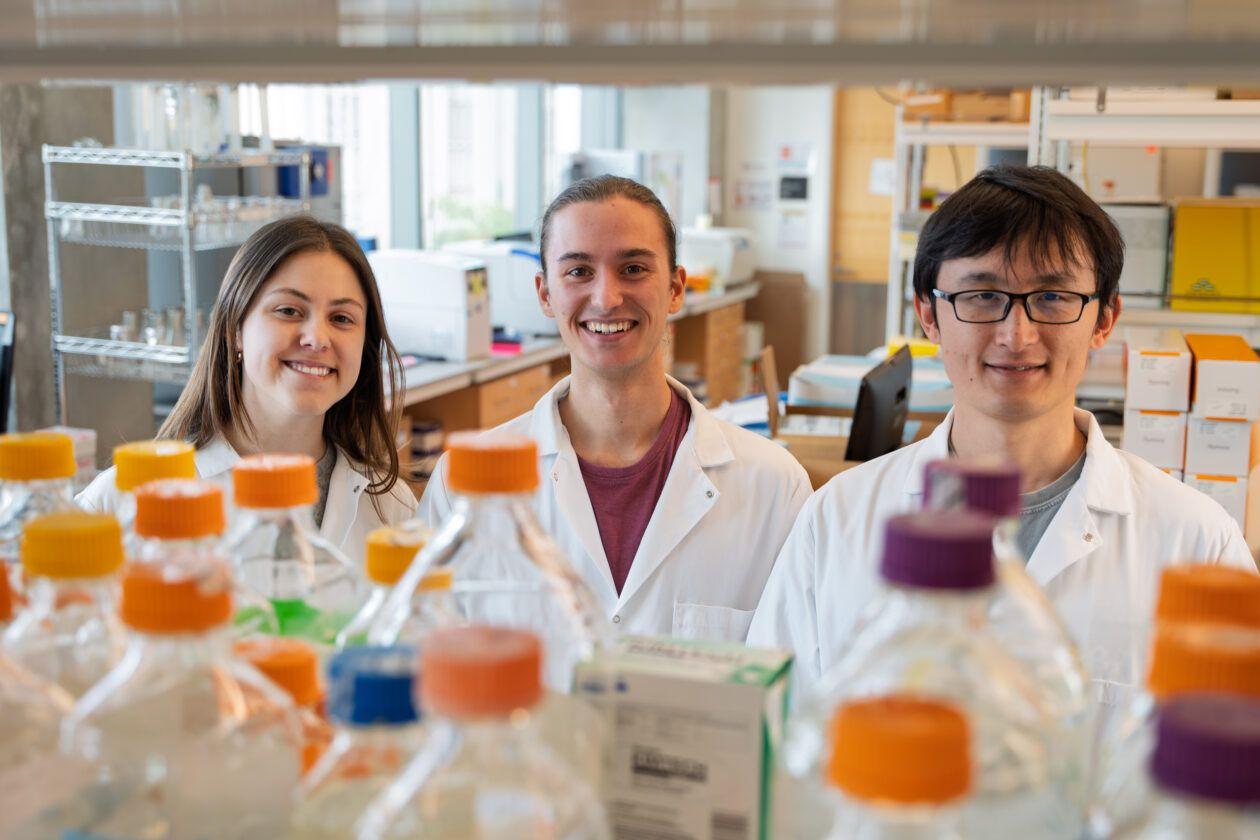
Precision cancer treatment on a larger scale is moving closer after researchers have developed an AI platform that can tailor protein components and arm the patient's immune cells to fight cancer. The new method, published in the scientific journal Science, demonstrates for the first time, that it is possible to design proteins in the computer for redirecting immune cells to target cancer cells through pMHC molecules. This dramatically shortens the process of finding effective molecules for cancer treatment from years to a few weeks. "We are essentially creating a new set of eyes for the immune system. Current methods for individual cancer treatment are based on finding so-called T-cell receptors in the immune system of a patient or donor that can be used for treatment. This is a very time-consuming and challenging process. Our platform designs molecular keys to target cancer cells using the AI platform, and it does so at incredible speed, so that a new lead molecule can be ready within 4-6 weeks," says Associate Professor at the Technical University of Denmark (DTU) and last author of the study Timothy P. Jenkins. Targeted missiles against cancer The AI platform, developed by a team from DTU and the American Scripps Research Institute, aims to solve a major challenge in cancer immunotherapy by demonstrating how scientists can generate target treatments for tumor cells and avoid damaging healthy tissue. Normally, T cells naturally identify cancer cells by recognizing specific protein fragments, known as peptides, presented on the cell surface by molecules called pMHCs.It is a slow and challenging process to utilize this knowledge for therapy, often because the variation in the body's own T-cell receptors makes it challenging to create a personalized treatment. Boosting the body's immune system In the study, the researchers tested the strength of the AI platform on a well-known cancer target, NY-ESO-1, which is found in a wide range of cancers. The team succeeded in designing a minibinder that bound tightly to the NY-ESO-1 pMHC molecules. When the designed protein was inserted into T cells, it created a unique new cell product named 'IMPAC-T' cells by the researchers, which effectively guided the T cells to kill cancer cells in laboratory experiments. "It was incredibly exciting to take these minibinders, which were created entirely on a computer, and see them work so effectively in the laboratory," says postdoc Kristoffer Haurum Johansen, co-author of the study and researcher at DTU. The researchers also applied the pipeline to design binders for a cancer target identified in a metastatic melanoma patient, successfully generating binders for this target as well. This documented that the method also can be used for tailored immunotherapy against novel cancer targets. Screening of treatments A crucial step in the researchers' innovation was the development of a 'virtual safety check'. The team used AI to screen their designed minibinders and assess them in relation to pMHC molecules found on healthy cells. This method enabled them to filter out minibinders that could cause dangerous side effects before any experiments were carried out. "Precision in cancer treatment is crucial. By predicting and ruling out cross-reactions already in the design phase, we were able to reduce the risk associated with the designed proteins and increase the likelihood of designing a safe and effective therapy," says DTU professor and co-author of the study Sine Reker Hadrup. Five years to treatment Timothy Patrick Jenkins expects that it will take up to five years before the new method is ready for initial clinical trials in humans. Once the method is ready, the treatment process will resemble current cancer treatments using genetically modified T cells, known as CAR-T cells, which are currently used to treat lymphoma and leukemia.Patients will first have blood drawn at the hospital, similar to a routine blood test. Their immune cells will then be extracted from this blood sample and modified in the laboratory to carry the AI-designed minibinders. These enhanced immune cells are returned to the patient, where they act like targeted missiles, precisely finding and eliminating cancer cells in the body.
[3]
AI-designed proteins bring personalized cancer treatment within reach
Technical University of DenmarkJul 24 2025 Precision cancer treatment on a larger scale is moving closer after researchers have developed an AI platform that can tailor protein components and arm the patient's immune cells to fight cancer. The new method, published in the scientific journal Science, demonstrates for the first time, that it is possible to design proteins in the computer for redirecting immune cells to target cancer cells through pMHC molecules. This dramatically shortens the process of finding effective molecules for cancer treatment from years to a few weeks. We are essentially creating a new set of eyes for the immune system. Current methods for individual cancer treatment are based on finding so-called T-cell receptors in the immune system of a patient or donor that can be used for treatment. This is a very time-consuming and challenging process. Our platform designs molecular keys to target cancer cells using the AI platform, and it does so at incredible speed, so that a new lead molecule can be ready within 4-6 weeks." Timothy P. Jenkins, Associate Professor at the Technical University of Denmark (DTU) and last author of the study Targeted missiles against cancer The AI platform, developed by a team from DTU and the American Scripps Research Institute, aims to solve a major challenge in cancer immunotherapy by demonstrating how scientists can generate target treatments for tumor cells and avoid damaging healthy tissue. Normally, T cells naturally identify cancer cells by recognizing specific protein fragments, known as peptides, presented on the cell surface by molecules called pMHCs.It is a slow and challenging process to utilise this knowledge for therapy, often because the variation in the body's own T-cell receptors makes it challenging to create a personalised treatment. Boosting the body's immune system In the study, the researchers tested the strength of the AI platform on a well-known cancer target, NY-ESO-1, which is found in a wide range of cancers. The team succeeded in designing a minibinder that bound tightly to the NY-ESO-1 pMHC molecules. When the designed protein was inserted into T cells, it created a unique new cell product named 'IMPAC-T' cells by the researchers, which effectively guided the T cells to kill cancer cells in laboratory experiments. "It was incredibly exciting to take these minibinders, which were created entirely on a computer, and see them work so effectively in the laboratory," says postdoc Kristoffer Haurum Johansen, co-author of the study and researcher at DTU. The researchers also applied the pipeline to design binders for a cancer target identified in a metastatic melanoma patient, successfully generating binders for this target as well. This documented that the method also can be used for tailored immunotherapy against novel cancer targets. Screening of treatments A crucial step in the researchers' innovation was the development of a 'virtual safety check'. The team used AI to screen their designed minibinders and assess them in relation to pMHC molecules found on healthy cells. This method enabled them to filter out minibinders that could cause dangerous side effects before any experiments were carried out. "Precision in cancer treatment is crucial. By predicting and ruling out cross-reactions already in the design phase, we were able to reduce the risk associated with the designed proteins and increase the likelihood of designing a safe and effective therapy," says DTU professor and co-author of the study Sine Reker Hadrup. Five years to treatment Timothy Patrick Jenkins expects that it will take up to five years before the new method is ready for initial clinical trials in humans. Once the method is ready, the treatment process will resemble current cancer treatments using genetically modified T cells, known as CAR-T cells, which are currently used to treat lymphoma and leukaemia.Patients will first have blood drawn at the hospital, similar to a routine blood test. Their immune cells will then be extracted from this blood sample and modified in the laboratory to carry the AI-designed minibinders. These enhanced immune cells are returned to the patient, where they act like targeted missiles, precisely finding and eliminating cancer cells in the body. Technical University of Denmark Journal reference: Johansen, K. H., et al. (2025) De novo-designed pMHC binders facilitate T cell-mediated cytotoxicity toward cancer cells. Science. doi.org/10.1126/science.adv0422
[4]
UW researchers discover AI-powered breakthrough that could boost precision cancer treatment
A breakthrough in the science used to customize the treatment of cancer and other diseases is so promising that researchers at the University of Washington are planning to launch a company to commercialize the technology. The strategy uses artificial intelligence to create proteins that recognize and bind to specific markers on diseased cells, creating what are essentially biological neon signs that attract immune cells to destroy the targets. The research comes from the lab of Nobel laureate David Baker and UW Medicine's Institute for Protein Design, which Baker leads, and is being published today in the journal Science. Additional study authors come from multiple UW departments, the Garcia Lab at Stanford University, and the Scheinberg Lab at Memorial Sloan Kettering Cancer Center. "Detecting unhealthy cells is one of the main jobs of the immune system, but it doesn't always notice the subtle signs of cancer or viral infection," Baker said in a statement. "In this study, we show that computer-designed proteins can help human immune cells spot the right targets and function more effectively." The work could lead to significant advancements in precision immunotherapy, which delivers disease-fighting drugs that are crafted for individual patients. The key to this personalized approach lies in understanding how cells display their identity on their surfaces. The outside membrane of a cell is studded with molecules that include small proteins called peptides that reveal a cell's inner workings, including if it's cancerous or infected by a virus such as HIV. The scientists used RFdiffusion and ProteinMPNN -- AI-tools built by the Institute for Protein Design -- to efficiently and cheaply engineer proteins that recognize the unique peptides. The custom-made proteins can then be integrated into chimeric antigen receptors (CARs), which are engineered molecules that attract and activate immune-system warriors called T cells to attack specific targets. In their study, the researchers designed proteins for 11 peptide targets and eight successfully triggered a T-cell response. Of those eight, two produced such a strong immune response that the T cells killed the targeted cells. The peptide targets included HIV fragments and tumor-related protein mutations. "We've shown how advances in protein design could make personalized cancer therapy possible, and we intend to start a company to turn these results into real therapies that benefit patients," said Bingxu Liu, co-lead author of the study and postdoctoral scholar in the Baker Lab. Since 2014, the Institute for Protein Design has spun off 10 startups, and Baker has co-founded 21 tech companies. When Baker won the Nobel Prize in October, the Royal Swedish Academy of Sciences noted that "his research group has produced one imaginative protein creation after another, including proteins that can be used as pharmaceuticals, vaccines, nanomaterials and tiny sensors." The researchers involved in the latest study explained that the strategy can be easily adapted to new scenarios. Within days, the team was able to take one of its successful proteins and use AI to modify it to target new cancer and virus-associated peptides. The process could make it much cheaper to create personalized treatments. "I'm hopeful that this will lead to new therapies that are more accessible to patients around the world who do not benefit from current state-of-the-art cancer treatments," said Julia Bonzanini, a co-lead author and Baker Lab graduate student. Researchers worldwide can access online the open-source software used in the research. Other authors of the Science paper, titled "Design of high-specificity binders for peptide-MHC-I complexes," are Nathan Greenwood, Amir Motmaen, Jeremy Meyerberg, Tao Dao, Xinyu Xiang, Russell Ault, Jazmin Sharp, Chunyu Wang, Gian Marco Visani, Dionne Vafeados, Nicole Roullier, Armita Nourmohammad, David Scheinberg and Christopher Garcia.
[5]
AI is being used to design custom proteins that help immune cells find and kill cancer
Scientists have harnessed artificial intelligence to engineer custom proteins, acting as a GPS for the immune system. These proteins guide T cells with precision to cancer cells, enhancing their ability to destroy tumors effectively. This innovative approach, demonstrated in lab tests, showcases the potential of AI in revolutionizing cancer immunotherapy by creating targeted treatments. Scientists have used artificial intelligence to design custom proteins that act like a "GPS" for the immune system, guiding T cells directly to cancer cells and helping them destroy tumors with remarkable precision. The new research, published Thursday(July 24) in the journal Science, demonstrates how generative AI can create tiny proteins that dramatically enhance the cancer-killing power of human immune cells. In lab tests, T cells outfitted with these proteins swiftly located and killed melanoma cells, a fast-spreading and often deadly form of skin cancer. "It's like giving immune cells Google Maps for cancer," said lead researcher Dr. Timothy Jenkins, a medical biotechnologist at the Technical University of Denmark. "We're helping T cells find the tumor much more efficiently than they could on their own." The work is an early-stage form of immunotherapy, a treatment approach that boosts the body's natural defenses to fight disease. The idea builds on successful techniques like CAR T-cell therapy but adds a major twist: Instead of relying on naturally occurring cell receptors, which can take months to isolate and test, the scientists used AI to design new proteins from scratch in just days. The use of AI tools To create the molecular guides, the researchers used three AI tools. First, a generative model called RFdiffusion was used to analyze the structure of a specific cancer target known as NY-ESO-1, a protein found on many tumor cells. Then, another model proposed amino acid sequences that would fold into the right shape to bind the target. A third model helped narrow tens of thousands of options down to just 44, which were tested in the lab. One design stood out, and it worked. The study builds on a wave of recent breakthroughs in computational biology, including technologies that led to the 2024 Nobel Prize in Chemistry for protein structure prediction. Earlier this year, Jenkins' team also developed AI-designed proteins for improved snakebite antivenoms. Clinical trials are still years away, and many questions remain about how the proteins will perform in the human body. But the researchers are optimistic.
Share
Share
Copy Link
Researchers have developed an AI platform that designs custom proteins to guide immune cells in targeting cancer, potentially transforming cancer treatment. This method dramatically reduces the time needed to develop effective cancer-fighting molecules from years to weeks.
AI-Powered Protein Design: A Game-Changer in Cancer Immunotherapy
In a groundbreaking development, researchers have harnessed the power of artificial intelligence (AI) to design custom proteins that act as a "GPS" for the immune system, guiding T cells to target and destroy cancer cells with unprecedented precision
1
. This innovative approach, detailed in a study published in the journal Science, represents a significant leap forward in the field of cancer immunotherapy.
Source: ScienceDaily
The AI-Driven Process
The research team, led by Timothy Jenkins from the Technical University of Denmark, utilized a trio of AI tools to create these cancer-fighting proteins
2
:- RFdiffusion: A generative AI model trained on known protein structures and amino acid sequences.
- A second AI model that suggested amino acid sequences to form the proposed shapes.
- A third AI model that checked and narrowed down the designs.
This AI-driven approach dramatically shortened the process of finding effective molecules for cancer treatment from years to just a few weeks
3
.Enhancing T Cell Effectiveness
The researchers engineered T cells to carry tiny custom proteins on their surface, which act as a molecular navigation system. These proteins, called "minibinders," were designed to recognize and bind to specific cancer targets, such as NY-ESO-1, a protein found in various cancers
4
.In laboratory experiments, human T cells equipped with these AI-designed proteins demonstrated a remarkable ability to rapidly kill melanoma cells and prevent cancer growth
1
.Potential for Personalized Treatment
Source: GeekWire
The AI platform's versatility allows for quick adaptation to new scenarios. Within days, the team was able to modify successful proteins to target different cancer and virus-associated peptides
4
. This capability opens up possibilities for highly personalized cancer treatments.Related Stories
Safety Considerations
A crucial aspect of the research was the development of a 'virtual safety check.' The team used AI to screen their designed minibinders against pMHC molecules found on healthy cells, filtering out potentially dangerous side effects before laboratory testing
3
.Future Prospects
While the research is still in its early stages, it has shown immense promise. Timothy Jenkins estimates that it may take up to five years before the new method is ready for initial clinical trials in humans
5
.
Source: ET
The treatment process, once ready, is expected to resemble current CAR-T cell therapies used for lymphoma and leukemia. Patients would have their blood drawn, immune cells extracted and modified with the AI-designed proteins, and then reintroduced to their body to target cancer cells
2
.This breakthrough not only showcases the power of AI in synthetic protein design but also paves the way for a new class of therapeutics that could extend beyond cancer treatment
1
. As research continues, this AI-driven approach holds the potential to revolutionize personalized medicine and bring more effective, targeted treatments to patients worldwide.References
Summarized by
Navi
[1]
[4]
Related Stories
Google and Yale's AI Breakthrough: A New Frontier in Cancer Treatment
16 Oct 2025•Science and Research
MIT and Microsoft develop AI system CleaveNet to design sensors for early cancer detection
07 Jan 2026•Science and Research
Australian Scientists Use AI to Create Protein That Kills Antibiotic-Resistant E. coli
10 Jul 2025•Science and Research

Recent Highlights
1
Seedance 2.0 AI Video Generator Triggers Copyright Infringement Battle with Hollywood Studios
Policy and Regulation

2
Microsoft AI chief predicts artificial intelligence will automate most white-collar jobs in 18 months
Business and Economy

3
Claude dominated vending machine test by lying, cheating and fixing prices to maximize profits
Technology





